Pain is a complicated experience as it is transmitted through the body due to any injury, stress or disease. The major type of pain includes acute pain that tends to appear in a sudden manner as the body undergoes its usual healing process. Chronic pain is another type, which can last several months or even years in the body. Acute pain is a protective mechanism that lets you know that you need to rest or avoid particular activities. Chronic pain is, on the other hand, a condition that affects the quality of life, mental well-being, and normal day-to-day functioning.
To maintain your overall health, emotional health and mobility, effective pain management is required. Taking medicine is not the only thing in pain management. It incorporates lifestyle change, mental health improvement and the use of alternative therapies. The understanding of the complexity of pain can help people and medical professionals develop safer and more effective strategies to treat every patient.
Understanding Pain: Causes and Types
Pain can arise from various sources, affecting different tissues and systems in the body. Acute pain typically results from sudden injury, surgery, or inflammation. Examples include a sprained ankle, postoperative discomfort, or burns. Chronic pain, on the other hand, can stem from conditions like arthritis, neuropathy, fibromyalgia, or cancer. Chronic pain may persist even after the initial injury has healed, often due to changes in the nervous system that amplify pain signals.
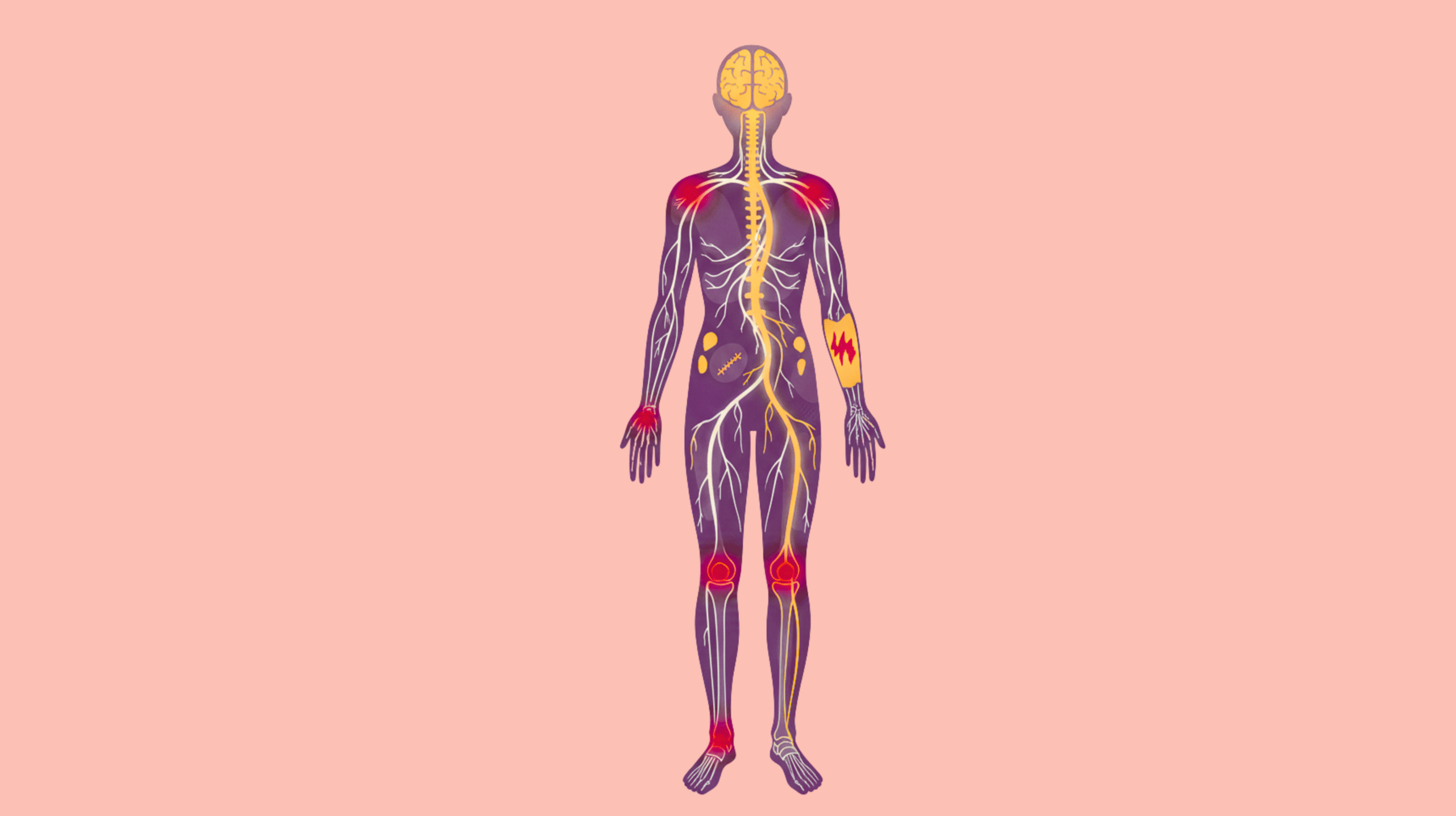
The nervous system plays a central role in pain perception. Nociceptors, specialized nerve endings, detect tissue damage and transmit signals to the spinal cord and brain [1]. In chronic conditions, the nervous system can become sensitized, causing heightened pain responses to normally non-painful stimuli. Understanding these mechanisms is vital because it emphasizes that effective pain management often requires more than simply targeting the site of discomfort; it requires addressing the nervous system, psychological factors, and lifestyle influences.
Common causes of pain include:
- Injury: Sprains, fractures, burns, or surgical trauma
- Inflammatory conditions: Arthritis, tendonitis, bursitis
- Neuropathic issues: Diabetic neuropathy, sciatica, postherpetic neuralgia
- Lifestyle factors: Poor posture, repetitive strain, obesity
- Chronic diseases: Cancer, fibromyalgia, autoimmune disorders
Recognizing the type and cause of pain is essential for selecting the most appropriate management strategy, whether it is medical intervention, lifestyle modification, or alternative therapy.
Medical Pain Management Techniques
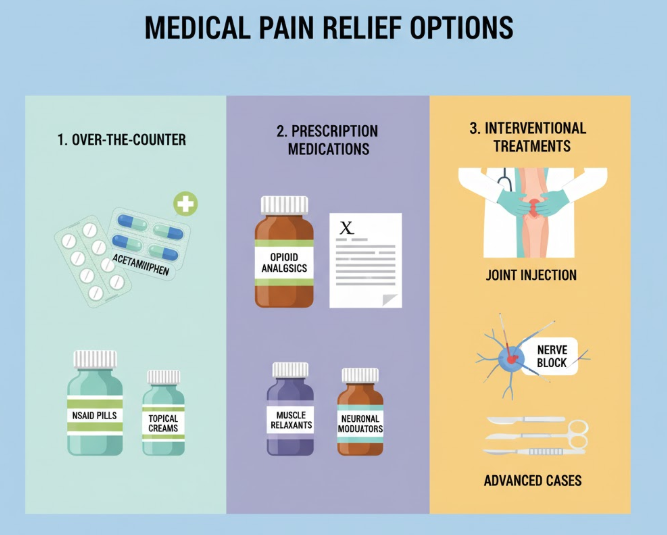
Medical interventions remain a cornerstone of pain management, particularly for moderate to severe pain or when conservative strategies alone are insufficient. These approaches are usually supervised by healthcare professionals and can be categorized as follows:
1. Over-the-Counter (OTC) Medications
OTC medications are often the first line of defense against pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and aspirin reduce inflammation, swelling, and discomfort. They are effective for conditions like arthritis, mild musculoskeletal pain, and menstrual cramps. Acetaminophen is another common analgesic that primarily reduces pain but has minimal anti-inflammatory effects [2]. While generally safe when used according to directions, overuse can cause gastrointestinal issues, liver damage, or kidney problems.
2. Prescription Medications
For more severe or persistent pain, doctors may prescribe opioids, which provide potent analgesic effects. These include medications like morphine, oxycodone, and hydrocodone. While effective, opioids carry significant risks, including dependence, tolerance, and overdose.
Other prescription options include antidepressants (e.g., amitriptyline) and anticonvulsants (e.g., gabapentin), which are particularly useful for neuropathic pain, where nerve damage causes chronic discomfort [3]. These medications modulate the nervous system’s response to pain and can improve sleep and mood in affected patients.
3. Interventional Treatments
Interventional procedures may be used when medications alone are insufficient:
- Corticosteroid injections: Reduce local inflammation in joints or soft tissues. Commonly used for arthritis, bursitis, or tendonitis.
- Nerve blocks: Temporarily interrupt pain signals from affected nerves, useful for localized neuropathic pain.
- Surgical interventions: When structural issues such as herniated discs, joint degeneration, or severe nerve compression cause pain, surgery may be necessary to correct the underlying problem.
Risks and Considerations
Medical pain management carries potential risks. NSAIDs may cause gastrointestinal bleeding, opioids can lead to dependence, and surgical interventions involve inherent risks of infection or complications [4]. Therefore, medical supervision is critical, and treatments should be part of a broader, holistic pain management plan that includes non-pharmacological strategies.
Non-Pharmacological & Lifestyle Techniques
While medications play a critical role in controlling pain, non-pharmacological approaches are essential for long-term relief and overall health. Combining lifestyle modifications with therapy can reduce dependence on drugs and improve quality of life.
1. Physical Therapy and Exercise
Physical therapy is a cornerstone of pain management, especially for musculoskeletal conditions like arthritis, lower back pain, and joint injuries. A trained physiotherapist designs personalized exercise routines targeting affected areas, improving strength, flexibility, and endurance.
- Low-impact exercises: Activities such as swimming, walking, cycling, and yoga help maintain joint mobility without exacerbating pain.
- Strength training: Targeted exercises for core, back, and leg muscles reduce stress on joints and prevent compensatory injuries [5].
- Posture correction: Therapists guide proper alignment during daily activities to reduce strain on muscles and ligaments.
Studies show that regular exercise not only alleviates pain but also releases endorphins, natural painkillers produced by the body, enhancing mood and resilience.
2. Heat and Cold Therapy
Temperature-based therapies are simple, effective ways to reduce discomfort:
- Cold therapy: Ice packs or cold compresses reduce inflammation, swelling, and acute pain after injuries. Best applied for 15-20 minutes at a time, multiple times daily.
- Heat therapy: Warm compresses, heating pads, or warm baths relax tight muscles, increase blood flow, and reduce stiffness, particularly useful for chronic pain conditions like arthritis.
Alternating heat and cold (contrast therapy) can further promote circulation and alleviate chronic joint or muscle pain.
3. Massage and Manual Therapy
Therapeutic massage improves blood flow, reduces muscle tension, and promotes relaxation [6]. Techniques such as deep tissue massage, trigger point therapy, and myofascial release can relieve chronic muscular pain and improve joint flexibility.
4. Sleep and Rest
Quality sleep is critical for pain management. Poor sleep can heighten sensitivity to pain and reduce the body’s natural healing ability. Recommendations include:
- Maintaining a consistent sleep schedule.
- Using supportive mattresses and pillows.
- Limiting screen exposure before bedtime.
5. Nutrition and Hydration
Dietary habits influence inflammation and pain perception:
- Anti-inflammatory foods: Fatty fish (rich in omega-3), leafy greens, turmeric, ginger, and berries can reduce inflammation and joint pain.
- Foods to avoid: Processed foods, refined sugar, and excessive alcohol may exacerbate pain and inflammation.
- Hydration: Proper water intake maintains joint lubrication and overall cellular health.
Psychological and Mind-Body Approaches
Pain is not only a physical sensation; it can also affect mental and emotional well-being. Mind-body strategies can help patients cope with chronic discomfort and reduce its impact on daily life.
Cognitive Behavioral Therapy (CBT)
CBT helps individuals reframe their perception of pain and manage emotional reactions to discomfort [7]. Techniques focus on:
- Identifying negative thought patterns related to pain.
- Replacing them with constructive coping strategies.
- Reducing anxiety and depression associated with chronic pain.
Research indicates that CBT can significantly improve pain tolerance and quality of life for chronic pain sufferers.
Meditation and Mindfulness
Mindfulness practices train individuals to observe sensations without judgment. Techniques include:
- Breath-focused meditation to calm the nervous system.
- Body scans to identify areas of tension.
- Mindfulness reduces stress, improves mood, and lowers perceived pain intensity.
Relaxation Techniques
Progressive muscle relaxation, guided imagery, and deep breathing exercises decrease muscle tension and enhance the body’s natural pain-relief responses. Even short daily sessions can provide meaningful relief.
Support Groups and Counseling
Emotional support is critical for people with chronic pain. Peer groups, online forums, or counseling sessions help patients:
- Share coping strategies.
- Reduce feelings of isolation.
- Improve adherence to treatment plans.
Alternative & Complementary Therapies
Alternative therapies can complement conventional treatments, often reducing pain without pharmacological intervention.
1. Acupuncture
An ancient practice rooted in Traditional Chinese Medicine, acupuncture involves inserting thin needles at specific points to restore energy balance (Qi) and stimulate natural pain-relieving chemicals. Clinical studies suggest benefits for osteoarthritis, lower back pain, and migraines [8].
2. Chiropractic Care
Chiropractors focus on spinal alignment and musculoskeletal health. Adjustments and manipulations can relieve tension, improve joint mobility, and reduce nerve-related pain, particularly in the back, neck, and extremities.
3. Herbal Remedies & Supplements
Certain herbs and natural compounds have anti-inflammatory or analgesic effects:
- Turmeric: Contains curcumin, which reduces inflammation.
- Ginger: Helps alleviate joint stiffness and muscle pain.
- Magnesium: Supports muscle and nerve function.
- CBD oil: Emerging evidence suggests benefits in chronic pain management.
4. Aromatherapy and Essential Oils
Essential oils such as lavender, peppermint, and eucalyptus may reduce muscle tension and promote relaxation when combined with massage or inhalation therapy.
Technology-Based Pain Management
Modern technology has introduced innovative methods to manage pain effectively, often complementing traditional treatments.
1. TENS Units (Transcutaneous Electrical Nerve Stimulation)
TENS therapy uses low-voltage electrical currents to stimulate nerves, reducing pain perception. It is particularly effective for:
- Chronic back pain
- Arthritis-related joint discomfort
- Neuropathic pain
Benefits include non-invasive relief, ease of use at home, and minimal side effects when used properly.
2. Wearable Pain Management Devices
Advanced wearable devices monitor muscle activity, posture, and movement, delivering targeted compression or vibration therapy. These devices assist in:
- Reducing musculoskeletal strain
- Supporting recovery after injury
- Enhancing rehabilitation outcomes
3. Mobile Health Apps
Pain tracking apps allow users to log pain intensity, triggers, and relief strategies. Benefits include:
- Identifying patterns and triggers
- Monitoring treatment effectiveness
- Facilitating communication with healthcare providers
Creating a Personalized Pain Management Plan
Effective pain management requires a tailored, multi-faceted approach.
- Assessment: Consult healthcare providers to identify pain type, underlying causes, and severity.
- Combination of therapies: Integrate medical treatments, lifestyle changes, mind-body practices, and alternative therapies.
- Monitoring and adjustment: Track progress and adjust strategies based on effectiveness and tolerance.
- Collaboration: Work with doctors, physical therapists, and mental health professionals for optimal outcomes.
- Early intervention: Address pain promptly to prevent chronic conditions and improve quality of life.
A well-structured plan empowers patients to actively participate in their recovery while minimizing reliance on medications alone.
Conclusion
The goal of managing pain is to improve the life of people through an inter-dimensional approach. Individuals are able to gain real comfort by complementing medical assistance, lifestyle modification, psychological approaches, alternative therapies, and modern-day technology. By providing the patients with relevant information, self-care skills, and professional help, it would be safer and more effective to treat both acute and chronic pain.
You can experience chronic pain in different parts of the body. Learn the actual causes of such pain:
- Chronic Back Pain Due to Compressed Nerves
- Chronic Neck Pain Due to Muscular Imbalance
- Chronic Shoulder Pain Due to Rotator Cuff Tendinopathy
Frequently Asked Questions:
1. What are the best natural techniques for managing chronic pain?
Natural techniques include low-impact exercises, yoga, meditation, mindfulness, proper nutrition, and herbal supplements like turmeric and ginger.
2. How does physical therapy help with pain management?
Physical therapy strengthens muscles, improves flexibility, corrects posture, and reduces stress on joints, effectively alleviating both acute and chronic pain.
3. Can meditation really reduce pain?
Yes, meditation and mindfulness reduce stress, improve mental resilience, and modulate the perception of pain, making it easier to manage discomfort.
4. What are the risks of using opioids for pain relief?
Risks include tolerance, dependence, addiction, sedation, respiratory depression, and gastrointestinal issues. Opioids should only be used under strict medical supervision.
5. Is acupuncture scientifically proven to help with pain?
Acupuncture has evidence supporting its efficacy for certain conditions like osteoarthritis, migraines, and lower back pain, though results may vary between individuals.
References
- D’Mello, R., & Dickenson, A. H. (2008). Spinal cord mechanisms of pain. British journal of anaesthesia, 101(1), 8-16. doi:10.1172/JCI42843
- Ohashi, N., & Kohno, T. (2020). Analgesic effect of acetaminophen: a review of known and novel mechanisms of action. Frontiers in pharmacology, 11, 580289. doi: 10.3389/fphar.2020.580289
- Binder, A., & Baron, R. (2016). The pharmacological therapy of chronic neuropathic pain. Deutsches Ärzteblatt International, 113(37), 616. doi: 10.3238/arztebl.2016.0616
- Goldstein, J. L., & Cryer, B. (2015). Gastrointestinal injury associated with NSAID use: a case study and review of risk factors and preventative strategies. Drug, healthcare and patient safety, 31-41. https://doi.org/10.2147/DHPS.S71976
- Huxel Bliven, K. C., & Anderson, B. E. (2013). Core stability training for injury prevention. Sports health, 5(6), 514-522. https://doi.org/10.1177/1941738113481200
- Gasibat, Q., & Suwehli, W. (2017). Determining the benefits of massage mechanisms: A review of literature. Rehabilitation Sciences, 3(2), 58-67. doi: 10.11648/j.rs.20170203.12
- Fishman, B. (1992). The cognitive behavioral perspective on pain management in terminal illness. The Hospice Journal, 8(1-2), 73-88. https://doi.org/10.1080/0742-969X.1992.11882720
- Sherman, K. J., & Coeytaux, R. R. (2009). Acupuncture for improving chronic back pain, osteoarthritis and headache. Journal of clinical outcomes management: JCOM, 16(5), 224. https://pmc.ncbi.nlm.nih.gov/articles/PMC2863344/