When you prepare your joints, limbs, prior to undergoing physiotherapy, the entire session becomes easier, with less pain, and more effective, particularly, in cases when you experience long-term pains or you are recovering from an injury. Only knowing all the things that are at play is not enough, it is mandatory to prepare your body. This is a step-by-step guide to the science and practice of preparing your joints to be used during physiotherapy with details.
Why Pre-Physiotherapy Joint Preparation Matters?
The Science Behind Pre-Session Joint Conditioning
Your joints work in properly tuned mechanisms which require a while to warm up before you can pick heavy objects. Research indicates that preconditioning, consisting of exercises that enhance scope of movements, and muscle strength around the joint reduces the perception of pain during the treatment, enhances the fluidity of the joints, and augments neuromuscular control [1]. Joint prep reduces inflammation indicators, and the prep initiates proprioceptive feedback. In other words, it makes your brain determine the location of your joints in space. This connection is quite crucial toward the prevention of the movement of people to help them compensate for the pain that might cause further worsening or result in additional injuries.
Common Joint Pain Reasons That Influence Therapy Effectiveness
Pain during therapy often roots in:
- Muscular weakness failing to support joints,
- Joint inflammation or swelling limiting movement [2],
- Stiffness from previous injury/fibrosis,
- Mechanical problems such as misalignment or instability.
Unaddressed, these reasons persist or worsen during therapy, reducing success rates. Preparing joints attempts to reverse or mitigate these factors beforehand.
Setting Realistic Expectations Through Proper Preparation
No magic pill here; preparation improves outcomes but requires consistency and realistic pacing. Understanding that joint prep stretches from gentle movement to targeted strengthening helps align expectations. You’re setting the stage, not performing a solo starring role yet.
Comprehensive Joint Assessment Prior to Physiotherapy
Testing Joint Range of Motion and Muscle Strength
First, you have to determine the position of your joint. Range of motion (ROM) tests determine the degree to which one can bend or straighten the joint without pain. Muscle strength tests, on the other hand, determine which supporting muscles are weak and require exercise prior to commencing rigorous therapy [3].
Therapists are able to prepare individualised prep plans using these tests and ensure that patients do not engage in exercises that may intensify their symptoms.
Detecting Swelling and Inflammation Early
A swelling joint means that it is inflamed and damaged. Therapists determine the degree of swelling by using tape measures or by looking at the appearance of the patient. Based on this knowledge, they adjust the level of treatment. Swollen joints do not react to strengthening exercises as well, and pain management is required prior to rehabilitation [4].
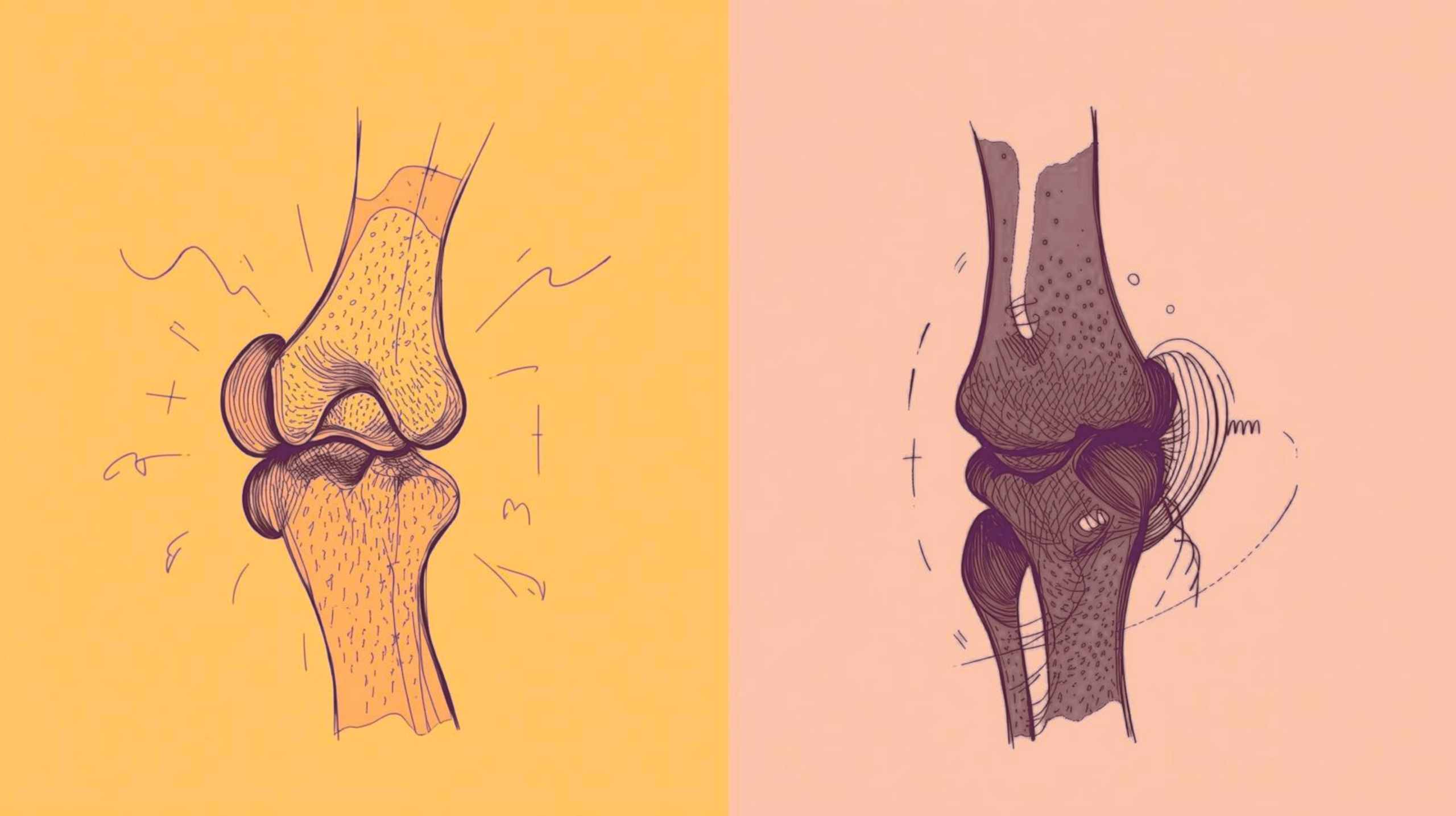
Utilizing Joint Pain Location Charts for Personalized Planning
Visual pain maps assist physicians in determining what areas within the joint require more focus; whether it is at the front, the middle, or the back and they can then indicate the certain pre-processed tasks that can withstand the therapy process better.
Exercises to Prime Joints for Physiotherapy Success

1. Gentle Stretching to Enhance Flexibility and Reduce Stiffness
- Quadriceps stretch: Stand, pull ankle towards buttock, hold 20 seconds.
- Hamstring stretch: Sit with one leg outstretched, reach towards toes.
- Calf stretch: Lean into a wall with one leg back, heel down.
These stretches promote flexibility without provoking pain, easing joint motion.
2. Isometric Strength Exercises to Activate Muscles Safely
- Quadriceps sets: Tighten thigh muscle, hold for 5-10 seconds.
- Glute squeezes: Contract buttocks muscles while seated or standing.
- Straight leg raises: Lift leg 6-12 inches while keeping knee straight.
Isometric moves fire muscles without joint strain, beneficial especially if swelling limits movement.
3. Low-Impact Cardiovascular Conditioning to Improve Endurance
- Walking on even surfaces.
- Swimming or water aerobics.
- Stationary cycling at low resistance.
These exercises promote blood flow, oxygen delivery, and joint nourishment, prepping you for more intense therapy.
4. Sample Routine for Pre-Physiotherapy Joint Prep
- Warm-up: 5-minute gentle walk.
- Stretching: 3-5 minutes of targeted muscle stretches.
- Isometric exercises: 2 sets of each muscle group, 10 reps.
- Low-impact cardio: 10 minutes swimming or cycling.
- Cool-down: Gentle stretching and relaxation for 2-3 minutes.
Consistency is key; 3-5 sessions weekly makes a meaningful impact.
Reducing Swelling and Managing Inflammation Before Sessions
Effective Cold Therapy and Compression Techniques
Cold packs reduce blood flow to inflamed areas, numbing pain and limiting swelling [5]. Apply an ice pack wrapped in a towel for 15-20 minutes per session, multiple times daily if needed.
Compression wraps or sleeves provide external pressure to curb fluid buildup and support joint structures during prep exercises.
Elevation and Natural Home Remedies for Joint Comfort
Elevate the joint above heart level to encourage venous return and reduce swelling. Herbal applications like turmeric paste or arnica cream may help symptomatically, though evidence is mixed; always consult your therapist or doctor.
When to Rest Versus When to Remain Active
Rest is essential during acute flare-ups; however, prolonged immobility weakens muscles and worsens stiffness. Monitor your pain and swelling levels, balancing rest with gentle movement.
Supportive Devices and Their Role in Joint Preparation
Selecting the Appropriate Braces and Supports
Braces vary in functionality; from elastic sleeves providing warmth and compression to hinged supports offering stability. Discuss with your physiotherapist to choose what suits your joint status best.
The Benefits of Compression Sleeves and Joint Caps
These assist with proprioception (joint awareness), reduce swelling, and provide reassuring support during pre-therapy movement.
Customized Orthotics and Mobility Aids: Pros and Cons
Orthotics can correct foot mechanics, improving joint alignment upstream [6]. However, improper use may create dependency or muscle weakness without parallel strengthening, so professional guidance matters.
Nutritional and Lifestyle Factors to Enhance Joint Health Before Therapy
Anti-Inflammatory Diet Basics Supporting Joint Recovery
Support healing with:
- Nuts, seeds, and oily fish rich in omega-3.
- Colorful fruits and vegetables packed with antioxidants.
- Spices like turmeric and ginger.
Avoid processed sugars and trans fats that may aggravate inflammation.
Importance of Hydration and Weight Management
Optimal hydration supports joint lubrication and toxin removal. Maintaining healthy weight reduces mechanical joint load, easing pain and improving therapy response.
Incorporating Mindfulness and Movement Awareness
Regular body scanning and technique focus during daily activities promote correct posture and reduce joint strain.
Psychological Preparation and Education Before Physiotherapy
Setting Realistic Expectations and Goals
Understanding that improvement is gradual fosters patience and motivation. Clear goal setting with your physiotherapist guides progress measurably.
Pain Coping Strategies to Improve Therapy Engagement
Breathing exercises, visualization, or listening to music during sessions can help manage discomfort, enhancing participation and performance [7].
The Role of Patient Education in Enhancing Outcomes
Informed patients adhere better to exercise programs, understand warning signs, and contribute actively to their recovery.
Monitoring Progress and Adjusting Preparation Techniques
1. Tracking Pain Levels and Joint Function Before Sessions
Use diaries or apps to record symptoms and any difficulties during prep exercises; valuable data for your care team.
2. How to Modify Pre-Exercise Routines Based on Feedback?
Flexibility to adapt intensity, duration, or type of exercises helps avoid exacerbation.
3. Collaborating with Your Physiotherapist for Personalized Prep Plans
Regular communication leads to tailored adjustments ensuring safety and efficacy.
Conclusion: The Road to Pain-Free Physiotherapy Sessions
Joint preparation prior to physiotherapy can make pain manageable. Lifestyle changes, tailor-made exercises, and the means of managing the swelling process may enable your joints to become stronger and more flexible and you will be able to withstand the challenges of the treatment.
Keep in mind that your joints do not hate you but they just want to be there with you. You can assist them (or lend them a brace) prior to the big day!
Joint pain can cause knee pain. Check how as well as its remedies:
Frequently Asked Questions:
1. What are the best exercises to prepare joints for physiotherapy?
Isometric exercises, gentle stretching, and low-impact cardio prime your joints effectively.
2. How can swelling be minimized before therapy sessions?
Cold therapy, compression, elevation, and rest in acute stages reduce swelling.
3. When should I use braces or supportive devices during preparation?
Use when pain or instability arises, but always under professional advice.
4. How does nutrition influence joint readiness for physiotherapy?
Anti-inflammatory, nutrient-rich foods support the healing environment.
5. What signs suggest adjustments are needed in my preparation routine?
Increased pain, swelling, or reduced function warrant modifying your plan.
References
- Boyd, L., Deakin, G. B., Devantier-Thomas, B., Singh, U., & Doma, K. (2023). The effects of pre-conditioning on exercise-induced muscle damage: a systematic review and meta-analysis. Sports Medicine, 53(8), 1537-1557. https://doi.org/10.1007/s40279-023-01839-8
- Palmer, T., & Toombs, J. D. (2004). Managing joint pain in primary care. The Journal of the American Board of Family Practice, 17(suppl 1), S32-S42. DOI: https://doi.org/10.3122/jabfm.17.suppl_1.S32
- Brown, L. E., & Weir, J. P. (2001). ASEP procedures recommendation I: accurate assessment of muscular strength and power. Journal of Exercise Physiology Online, 4(3). https://d1wqtxts1xzle7.cloudfront.net/38566621/Brown2001-libre.pdf?1440513021=&response-content-disposition=inline%3B+filename
- Howell, J. N., Chleboun, G., & Conatser, R. (1993). Muscle stiffness, strength loss, swelling and soreness following exercise‐induced injury in humans. The Journal of physiology, 464(1), 183-196. https://doi.org/10.1113/jphysiol.1993.sp019629
- Kuo, C. C., Lin, C. C., Lee, W. J., & Huang, W. T. (2013). Comparing the antiswelling and analgesic effects of three different ice pack therapy durations: a randomized controlled trial on cases with soft tissue injuries. Journal of Nursing Research, 21(3), 186-193. DOI: 10.1097/jnr.0b013e3182a0af12
- Mohaddis, M., Maqsood, S. A., Ago, E., Singh, S., Naim, Z., & Prasad, S. (2023). Enhancing functional rehabilitation through orthotic interventions for foot and ankle conditions: A narrative review. Cureus, 15(11). DOI: 10.7759/cureus.49103
- Osborne, M. S., Greene, D. J., & Immel, D. T. (2014). Managing performance anxiety and improving mental skills in conservatoire students through performance psychology training: a pilot study. Psychology of Well-being, 4(1), 18. https://doi.org/10.1186/s13612-014-0018-3