Achilles pain is one of those annoyingly common problems that people almost always just think they can “walk off”. until suddenly, they don’t. It generally dawns as a little stiffness near the heel in morning, or a tight pull after running, and then it quietly elevates to pain with stairs, jumping or even walking normally.
Part of the issue is that Achilles tendon problems tend to feel like they can be managed at first, and so they are ignored. But the Achilles tendon takes enormous loads, especially when you run, sprint, jump or do calf raises, and once it is irritated there is inevitably some smart and progressive rehab in your future, not random stretching despite pain.
In this article, we will cover the below:
- What Achilles tendonitis/tendinopathy actually is,
- Why stretching may work (and when it won’t),
- Best stretches and eccentrics for Achilles relief,
- Mistakes that slow healing,
and how you can support recovery outside of stretching (like posture and recovery habits that don’t feel stuffy).
Quick reminder: If you felt a sudden “pop,” are experiencing major swelling, can’t push off the foot or cannot walk normally, skip the stretches and get a medical evaluation.
Understanding Achilles Tendonitis
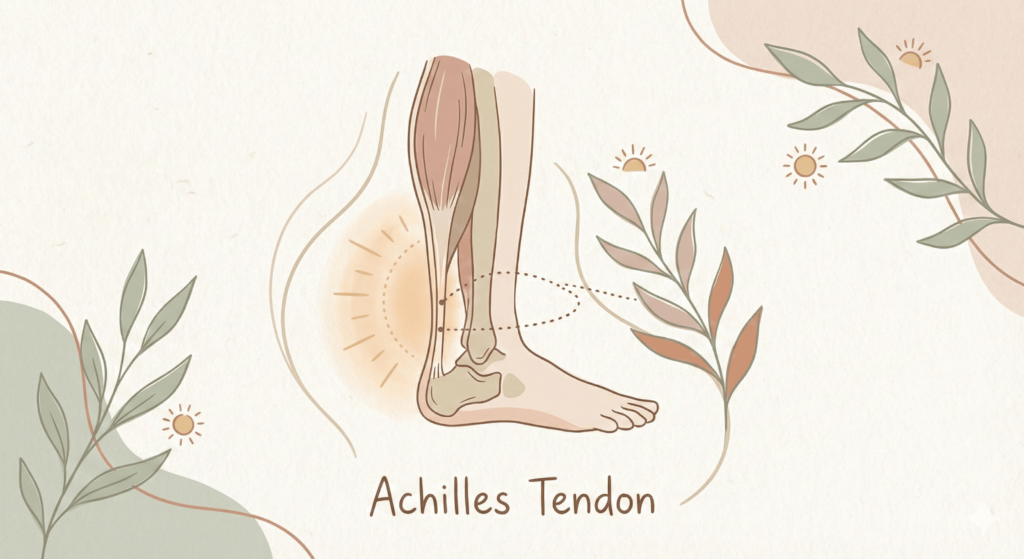
What does the Achilles tendon do ?
Your Achilles tendon attaches your calf muscles (gastrocnemius and soleus) to your heel bone. It really is the thick “power cable” that assists you:
Take off when walking or running, jump, climb stairs, and control ankle motion.
That’s why it is so easy to overload: It plays a role in nearly everything you do on your feet.
Tendonitis vs tendinopathy
You’ll hear people use the term “Achilles tendonitis,” but a lot of long-term cases are more appropriately termed Achilles tendinopathy ,a broader term that encompasses pain and degeneration-like changes in the tendon, as opposed to purely inflammatory processes.
According to studies, Achilles tendinitis as an overuse injury and highlights stretching and progressive strengthening as part of prevention and care.[1]
In plain language:
Tendonitis indicates a more inflamed, angry condition.
Tendinopathy is often an “angry tendon” process that reflects a longer-term load problem and hence needs more than just rest.
Common Causes of Achilles Pain
In most cases, Achilles pain can be boiled down to the tendon being asked to do more than it’s ready for suddenly or repeatedly.
1. Overuse
Over time, repetitive load (running volume, hill work, skipping, jumping) may irritate the tendon particularly with poor recovery.
2. Sudden training changes
- Big leaps in intensity are classic catalysts:
- increasing mileage too fast,
- adding speed work,
- starting plyometrics,
- switching to hills/stairs unexpectedly.
- Tight calves
So if your calves are tight, it can impede mobility in the ankle. That can put more strain on the Achilles in everyday movements. Stretching isn’t a cure-all, but calf mobility is frequently in the mix.
3. Poor footwear
Worn-out shoes, rapid transition to minimal footwear, or shoes that don’t suit your mechanics can alter tendon load. Depending on the issue in the Achilles, some rehab plans initially do use heel lifts as a temporary measure to decrease strain.
When Stretching Helps (and When It Doesn’t)
Stretching may help, but it’s far from the entire rehab.
Improving blood flow
A little bit of gentle stretching and movement will help with circulation in the lower leg. Tendons are not as rich in blood supply as muscles, so slow, gradual movement often feels better than total immobilization.
Reducing stiffness
Morning stiffness is a common complaint for people with Achilles issues. Soft mobility can alleviate that “first-step pain” sensation.
The missing piece: load management
Tight hamstrings or calf muscles aren’t necessarily the culprit of achy Achilles, stretching alone likely won’t fix it if your tendon is still being overloaded every day. Eccentrics and heavy slow resistance are often good at first with a cautious progression.
Research suggests that clinicians should consider the use of tendon loading exercise (ie, eccentric or heavy-load slow-speed training) as a first-line treatment for midportion Achilles tendinopathy.[2]
When stretching doesn’t help
Stretching can backfire if:
- You push into sharp pain,
- You pull at a reactive tendon with aggressive “yanking” stretches,
- You are experiencing insertional Achilles pain (pain right where the tendon attaches to heel bone) and you repeatedly drop your heel lower than a step edge.
As a general rule: keep stretching gentle, and treat strengthening/loading as the long-term builder.
Best Stretches To Relieve Achilles Tendon Pain (Safe + Effective)
Before you begin Relish feelings of mild discomfort, not burning pain. A practical rule is G, “comfortable stretch sensation” that disappears within 24 hours.
1. Standing calf stretch (gastrocnemius)
This is the classic wall stretch with a straight back knee. It addresses the gastrocnemius, which spans both knee and ankle.
How to do it
- Face a wall, hands on wall.
- Step the bad leg back, and pull that heel down toward the floor, keeping your knee straight.
- Lean slightly forward until you feel a stretch in the upper calf.
- Hold 30-45 seconds, 2-4 rounds.
- Form cues
- Press the back foot forward (do not allow it to flare open).
- Keep your heel down, heavy in the floor.
2. Seated towel stretch (gentle, adjustable)
It is a good choice for the mornings when my tendon feels stiff, and I want something more controlled.
How to do it
- Sit with your leg straight.
- Wrap a towel around the ball of your foot.
- And gently pull on the towel to help bring your toes toward you.
- Hold 30-45 seconds, 2-4 rounds.
Why it’s useful
- You can control intensity easily.
- It’s not as “bodyweight aggressive” as wall stretches.
3. Eccentric heel drops (the rehab standard)
Eccentric work refers to when a muscle is lengthening while under tension, think “slow lowering.” There is good evidence for this method to be effective in pain and function improvement for Achilles tendinopathy. A narrative review found that eccentric exercise was beneficial in clinical practice for the treatment of Achilles tendinopathy. [3]
How to do it
- Keep your feet out of the water and on the step you are standing on while holding on to a railing for support.
- Rise up with both feet.
- Load more to the sore side.
- Lower heel in 3–5 seconds.
- Sets/reps (starter-friendly)
- Begin with 2–3 sets of 8–12 repetitions, once a day, 3–5 days/week.
- Work your way up (more reps, then added load, as in a backpack).
Vital note Some reps will be very loud. But if it flares you, you don’t have to copy a “180 reps/day” model. Better to stay consistent and tolerable with a loading plan than to play the hero and chase pain.
4. Soleus-focused stretches (bent-knee calf stretch)
The deeper calf muscle, the soleus tends to be even more important for Achilles pain; at least, for pain while walking and for endurance.
How to do it
- A wall stretch like the above, but bend back knee a little while keeping heel down.
- You will be able to feel the stretch lower down in your calf, nearer to your Achilles.
- Hold 30-45 seconds, 2-4 rounds.
Why it matters
Stretch only with the knee straight, and you may overlook the soleus and your tendon may remain stiff.
Stretching Goof-ups to Avoid (These SLOWHEALING)
Aggressive bouncing
Jumping or bouncing stretches can inflame the tendon and turn up sensitivity to pain. Ligaments in general don’t respond well to that fast yank, but rather steady and controlled loading.
Stretching through sharp pain
A little discomfort is tolerable but sharp pain isn’t a good sign. And if you flare symptoms, you may find yourself caught in a cycle where each “stretch session” is a step backward.
Good checkpoint: when your pain/stiffness is significantly worse the next morning, you did too much.
Supporting Recovery Beyond Stretching (Where Most People Succeed or Fail)
Stretching helps, but Achilles recovery usually improves fastest when you treat it like a rebuild plan.
Rest vs active recovery
Full rest can calm things down short-term, but complete unloading often leads the tendon to being less tolerant when you come back. A more useful approach:
- Reduce the aggravating activity (like running volume),
- Keep pain-limited movement,
- Build tendon capacity with progressive strength.[4]
Footwear and heel support
Some practical tips that can make all the difference in real life :
- Wear supportive shoes during flare-ups. Walking on a hard floor isn’t going to help the pain at all, but you’ll feel better in supportive shoes so that your tendons aren’t so irritated as they gain strength back.
- Avoid sudden footwear transitions. Transitioning too suddenly to minimalist shoes can increase load on the achilles; if you’re going to make that transition, do so gradually and only when symptoms have stabilized.
- Consider temporary elevation of the heel if indicated. Some clinicians prescribe heel lifts to decrease compressive strain on the tendon in some cases (particularly insertional pain), but it’s a judgment call.
Compression and icing
These are symptom tools; helpful, but they aren’t the main cure.
- Ice after a flare-up. Icing can temporarily reduce pain sensation for some people, particularly where exercise is concerned, but it won’t “fix” the tendon on its own.
- Compression can soothe sore swelling feelings. A light compression sock or wrap could help make walking more comfortable as well shrink that “hot tendon” feeling.
Recovery Foundations for Achilles Pain: Posture, Sleep, and Tissue Calm
Here’s the quiet truth: It gets harder to rehab an Achilles when you’re not recovering well overall. Sleep, stress to your nervous system and overall stiffness all impact pain sensitivity.
Sleep posture matters for tissue recovery.
How we sleep matters for our tissue recovery. Your pain threshold frequently drops and your body recovers more slowly from sleep when you’re not snoozing well (neck tension, restless tossing). A supportive pillow that ensures your upper body stays comfortable can make the whole recovery process, because you do actually rest.
Support your “down time” posture
Support your “down time” posture.If you spend hours seated with poor posture, calves and ankles can stiffen up, and your overall movement quality drops. Betterhood’s posture-first mindset is basically: make the default positions (sleeping, sitting) less stressful so rehab can work
Recovery rituals make consistency easier
Recovery rituals make consistency easier. A bit of simple nightly mobilizing: light calf mobility, some gentle foot/ankle movement, and then relax helps you stay consistent enough in rehab to actually get results.
Conclusion
Achilles tendonitis/tendinopathy is commonplace, stubborn, and yet wickedly recoverable if you treat it like a slow rebuild. Do you need to stretch? While stretching can help decrease stiffness and increase mobility short-term, the real long term win is generally load management + progressive tendon loading like controlled eccentrics.
Most importantly: consistency beats intensity. Work the basics, don’t push too hard through sharp pain and give your tendon time to adapt. With patience and an intelligent plan, you can return to pain-free walking, running and training.
Explore More Health & Wellness Solutions:
Want to stay informed about wellness and everyday health issues? Here are some insightful reads to guide you. Explore the links below for practical tips and solutions.
- How to Prevent Knee Injuries: Proven Tips, and Lifestyle Strategies for Stronger Joints
- How Can Knee Cap Support Help Prevent Injury and Reduce Pain While Running
- 10 Effective Home Remedies for Body Pain Relief Naturally
Frequently Asked Questions:
1. How long does it take for Achilles tendonitis to heal?
Rehab time depends on the severity, load management and diligent rehab. In mild cases, it may reduce after a few weeks and with chronic Achilles tendinopathy, this could take several months. Progressive strengthening, not just rest, is essential for long-term recovery.
2. Is it a good idea for me to stretch my Achilles tendon daily?
Mild stretching can be performed on a daily basis as long as it does not produce any pain or only mild discomfort. But just stretching won’t do it. More lasting gains are made with daily tendon loading (eccentrics or slow resistance training).
3. Is it better to walk or rest for Achilles tendon pain?
Walking is generally safe and beneficial as long as one remains within pain-tolerant levels. Do not limp or work through sharp pain. Tolerable and supportive footwear, along with dose progressions of the load, enable movement whilst avoiding excessive stress to the tendon.
4. Which exercise is best for Achilles tendinopathy?
Eccentric exercises and heavy slow resistance are classified as level 1 evidence for mid-portion Achilles tendinopathy. These exercises ultimately re-educate the tendon to prepare for load and by progressively overloading progressing, they build your tendon strength by creating greater load tolerance.
5. What point should I stop stretching and go see a doctor for Achilles pain?
See a doctor if your pain is getting worse despite rehab, your swelling is improving and you still can’t walk normally or if you have sudden pain, weakness or popping. These symptoms could be a sign of a more serious injury that will likely require professional help.
References
- Cleveland Clinic. (n.d.). Tendonitis. https://my.clevelandclinic.org/health/diseases/10919-tendonitis
- Mayo Clinic. (n.d.). Achilles tendinitis—Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/achilles-tendinitis/symptoms-causes/syc-2036902
- de Vos, R.-J., van der Vlist, A. C., Winters, M., & Smithuis, F. J. (2012). A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. British Journal of Sports Medicine, 46(3), 214–218. https://doi.org/10.1136/bjsports-2011-090035
- Mayo Clinic. (n.d.). Achilles tendinitis—Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/achilles-tendinitis/symptoms-causes/syc-2036902
- Martin, R. L., et al. (2024). Achilles pain, stiffness, and muscle power deficits: Midportion Achilles tendinopathy revision 2024 (Clinical Practice Guideline). Journal of Orthopaedic & Sports Physical Therapy. https://www.jospt.org/doi/10.2519/jospt.2024.0302
- Murphy, M., Travers, M., Gibson, W., & Chivers, P. (2019). Eccentric exercise for Achilles tendinopathy: A narrative review and clinical decision-making considerations. Physical Therapy Reviews. https://pmc.ncbi.nlm.nih.gov/articles/PMC7739229/
- Silbernagel, K. G., Thomeé, R., Eriksson, B. I., & Karlsson, J. (2012). A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. British Journal of Sports Medicine, 46(3), 214–218. https://bjsm.bmj.com/content/46/3/214
- Rehab Hero. (n.d.). Wall calf stretch. https://www.rehabhero.ca/exercise/wall-calf-stretch
- NewYork-Presbyterian. (n.d.). Towel stretch. https://www.nyp.org/healthlibrary/multimedia/towel-stretch
- Rehab Hero. (n.d.). Bent knee calf stretch. https://www.rehabhero.ca/exercise/bent-knee-calf-stretch