Chronic knee pain is a widespread issue that affects millions globally, and one of the leading causes is osteoarthritis (OA), a degenerative joint condition. As people age, the knee joint becomes especially vulnerable due to its weight-bearing nature and repetitive use. This comprehensive guide explores osteoarthritis in the knee, including its causes, associated conditions, diagnosis, symptoms, treatment options, and prevention strategies to help manage the condition effectively.
What is Osteoarthritis in the Knee?
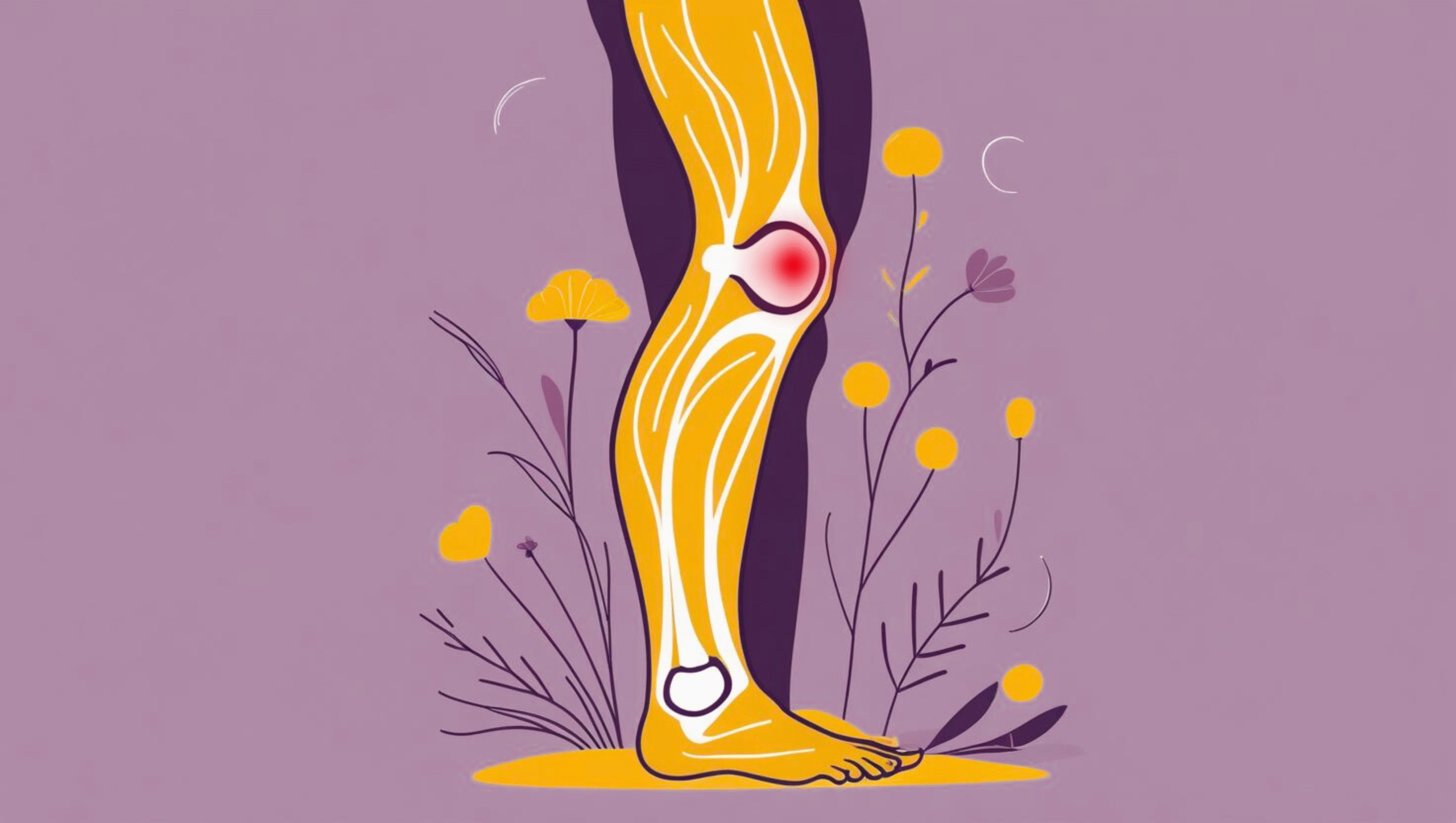
Osteoarthritis is a degenerative joint disease that primarily targets cartilage the smooth tissue covering the ends of bones within joints. In the knee, this cartilage ensures smooth, pain-free movement. However, due to factors like aging, repetitive stress, or trauma, the cartilage can begin to deteriorate.
As cartilage breaks down, bones in the knee begin to rub against each other, causing pain, stiffness, swelling, and reduced mobility. In severe cases, the condition can lead to bone spurs (osteophytes), which further impair joint movement and increase discomfort.
Causes of Osteoarthritis in the Knee
Understanding the contributing factors can help in preventing or managing OA:
- Aging: The most common risk factor. Cartilage naturally wears down with age.
- Obesity: Excess body weight puts increased pressure on knee joints, accelerating cartilage degeneration.
- Poor Posture & Weak Muscles: Misalignment and muscle imbalance lead to uneven stress on the knees.
- Repetitive Stress Injuries: Activities involving frequent knee bending, twisting, or high-impact sports increase risk.
- Previous Joint Injuries: Previous fractures, ligament damage, or meniscus injuries can predispose one to OA.
- Genetics: A family history of osteoarthritis may increase the likelihood of developing the condition.
Symptoms of Knee Osteoarthritis
The symptoms of OA can develop gradually and worsen over time:
- Pain: Especially during movement or after prolonged activity. In advanced stages, pain may persist even at rest.
- Stiffness: Usually felt in the morning or after sitting for long periods.
- Swelling: Caused by inflammation or excess fluid in the joint.
- Reduced Range of Motion: Difficulty in fully bending or straightening the knee.
- Crepitus: A grating or crunching sensation when moving the knee.
- Tenderness: The knee may feel sore when touched.
Health Conditions Associated with Knee OA
Osteoarthritis in the knee can exacerbate or be complicated by other health conditions:
- Meniscus Tears: Degenerative OA weakens the meniscus, making it prone to tears.
- Rheumatoid Arthritis: Coexisting autoimmune inflammation can worsen joint damage.
- Gout and Pseudogout: Crystal deposits in joints can lead to acute pain and swelling, often intensifying OA symptoms.
- Septic Arthritis: Infections in the joint, though rare, can co-occur and require immediate medical intervention.
Diagnosis of Osteoarthritis in the Knee
Clinical Examination
A healthcare provider will check for:
- Joint tenderness
- Swelling
- Range of motion
- Muscle strength and alignment
Imaging Tests
- X-rays: Show joint space narrowing, bone spurs, and changes in bone density.
- MRI Scans: Useful for assessing cartilage loss, meniscus damage, or soft tissue abnormalities.
Treatment Options for Knee Osteoarthritis
While there’s no cure, several strategies help reduce symptoms and improve function.
Lifestyle Modifications
- Exercise: Low-impact activities like swimming or cycling improve flexibility and strengthen muscles.
- Weight Loss: Reduces stress on the knees and slows down joint degradation.
Medications
- NSAIDs: Ibuprofen or naproxen to relieve pain and inflammation.
- Topical Analgesics: Pain-relieving creams and gels.
- Corticosteroid Injections: Short-term relief from severe inflammation.
- Hyaluronic Acid Injections: Improve joint lubrication and reduce pain.
Physical Therapy
- Strengthens quadriceps, hamstrings, and surrounding muscles.
- Improves balance and gait.
- Increases flexibility and reduces joint stiffness.
Support Devices
- Knee Braces: Provide joint support and correct alignment.
- Orthotics: Customized shoe inserts to reduce stress on knees.
- Canes or Walkers: Help redistribute weight and prevent further damage.
Surgical Options
- Arthroscopy: Minimally invasive; removes loose cartilage or bone fragments.
- Osteotomy: Realigns the bones to shift stress away from damaged areas.
- Partial Knee Replacement: Replaces only the damaged part.
- Total Knee Replacement: For severe cases, the entire knee joint is replaced with an artificial implant.
Diet and Supplements for Knee OA
Some dietary strategies and supplements can support joint health:
- Omega-3 Fatty Acids: Found in fish oil, they reduce inflammation.
- Vitamin D & Calcium: Strengthen bones.
- Glucosamine & Chondroitin: May help in cartilage repair and reduce symptoms.
- Antioxidant-rich foods: Berries, leafy greens, and nuts combat inflammation.
Prevention Strategies
Even if you’re at risk, certain actions can slow the onset or progression:
- Maintain Healthy Weight: Prevents unnecessary strain on knees.
- Engage in Regular Exercise: Focus on strength, flexibility, and low-impact cardio.
- Protect Your Joints: Use proper techniques while lifting or exercising.
- Stay Hydrated: Helps maintain joint lubrication.
- Avoid Repetitive Strain: Mix up activities and take frequent breaks.
Living with Knee Osteoarthritis
Living with chronic pain can be mentally and physically challenging. It’s important to:
- Set realistic goals for activity.
- Use assistive devices if needed.
- Seek support from physiotherapists, support groups, or counselors.
- Track progress and adjust treatment plans accordingly.
When to See a Doctor
Seek medical attention if:
- Pain interferes with daily activities
- You experience night pain or rest pain
- Swelling doesn’t subside with rest or medication
- There’s a sudden loss of mobility or function
Conclusion
Chronic knee pain due to osteoarthritis is a progressive condition, but it doesn’t have to take over your life. Early diagnosis, a well-rounded treatment approach, and lifestyle changes can significantly improve joint function and quality of life. Work closely with your healthcare provider to tailor a plan that suits your needs.
References
- Hunter, D. J., & Bierma‑Zeinstra, S. (2019). Osteoarthritis. The Lancet, 393(10182), 1745–1759. https://doi.org/10.1016/S0140‑6736(19)30417‑9
- StatPearls Contributors. (2024). Knee Osteoarthritis. StatPearls. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK507884/
- Spandidos Publications. (2023). Knee osteoarthritis: Current status and research progress. Experimental and Therapeutic Medicine, 21(1), Article 1. https://doi.org/10.3892/etm.2023.12180
- Frontiers in Medicine Editors. (2025). Recent advances in the management of knee osteoarthritis. Frontiers in Medicine, 12:1523027. https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1523027/full
- Radojcic, M. R., et al. (2019). Biomarker of extracellular matrix remodelling C1M and proinflammatory cytokine IL‑6 are related to synovitis and pain in end‑stage knee osteoarthritis patients. Preprint, arXiv. https://arxiv.org/abs/1903.10323
- Karsdal, M. A., et al. (2021). Multimodal Machine Learning‑based Knee Osteoarthritis Progression Prediction from Radiographs and Clinical Data. Preprint, arXiv. https://arxiv.org/abs/1904.06236
- ScienceDirect Authors. (2013). The epidemiology and impact of pain in osteoarthritis. ScienceDirect. https://www.sciencedirect.com/science/article/pii/S1063458413007607
- Pierce, E., & co‑authors. (2024). Chronic knee pain—diagnosis and evidence‑based management. Pain Practice, 25(3), 13408. https://onlinelibrary.wiley.com/doi/10.1111/papr.13408
- Health.com Editorial. (2023). What causes knee pain—and how to find relief. Health.com. https://www.health.com/knee-pain-8421212