Neck pain is a common complaint that affects millions of people worldwide, especially as they age. While neck pain can stem from poor posture, injury, or repetitive strain, one of the most common underlying causes in older adults is cervical osteoarthritis, also known as cervical spondylosis.
This article examines the role of osteoarthritis in causing chronic neck pain, the underlying biological mechanisms, and strategies for its identification, management, and prevention.
What Is Osteoarthritis of the Neck?
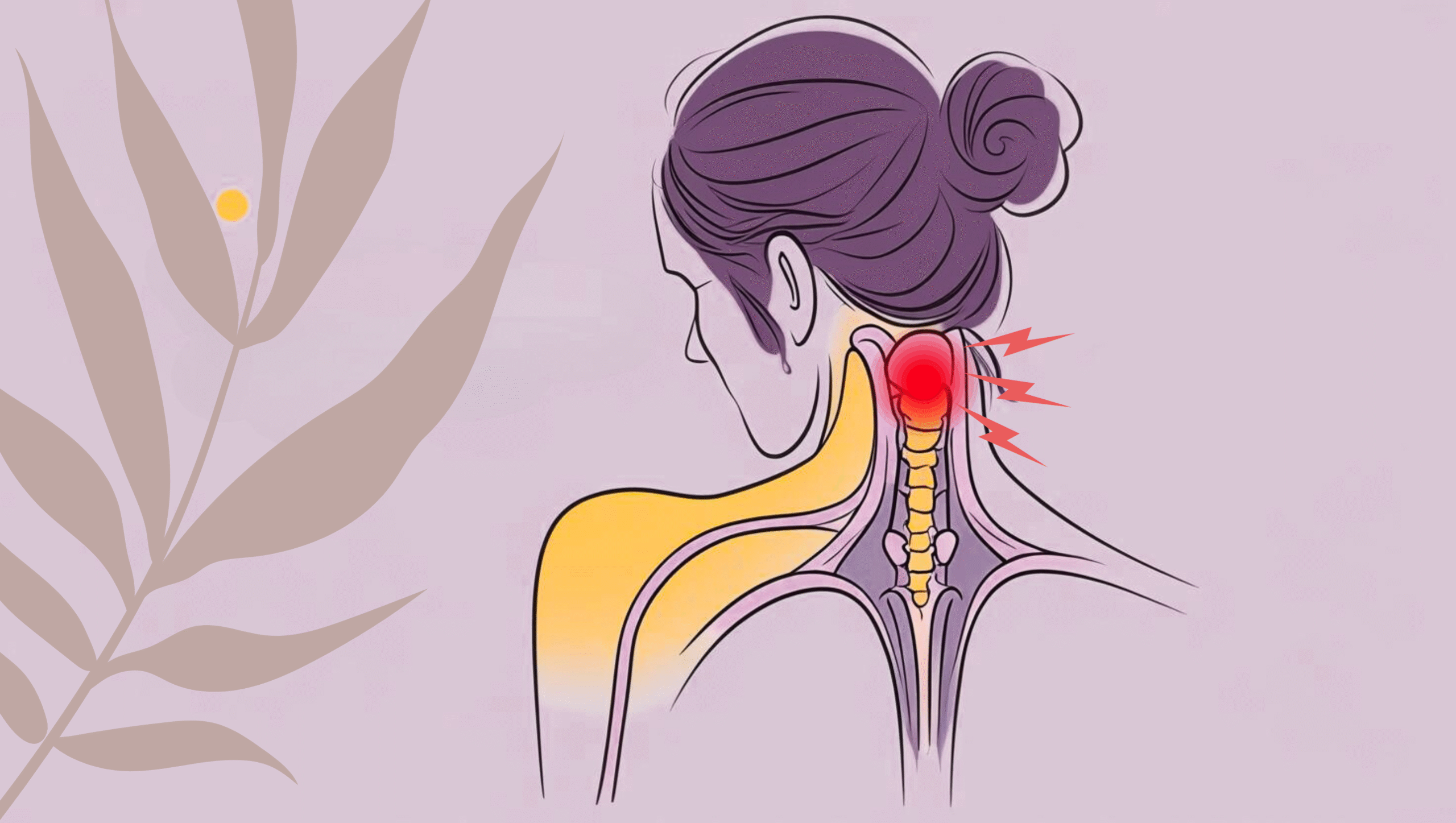
Osteoarthritis (OA) is a degenerative joint disease that occurs when the cartilage cushioning the ends of bones wears down over time. In the neck, this process affects the cervical spine — the top portion of the spinal column, composed of seven vertebrae (C1–C7).
When osteoarthritis affects the cervical spine, it leads to:
- Loss of cartilage between vertebrae
- Bone spurs (osteophytes) that form as the body attempts to repair damage
- Degeneration of intervertebral discs, leading to narrowing of disc space (disc height loss)
- Thickening of ligaments and possible nerve compression
All these structural changes can lead to chronic neck pain, stiffness, and even neurological symptoms.
How Osteoarthritis Causes Chronic Neck Pain
1. Degeneration of Cartilage
Cartilage serves as a shock absorber and enables smooth movement between vertebrae. In osteoarthritis, this cartilage breaks down, causing bones to rub together, which leads to inflammation and pain.
2. Disc Degeneration
The intervertebral discs between the vertebrae begin to dehydrate and shrink with age. This disc degeneration contributes to reduced cushioning, increasing friction between bones and resulting in pain and reduced mobility.
3. Bone Spurs and Nerve Compression
As a reaction to cartilage loss, the body may develop bony outgrowths (bone spurs) around the joints. These spurs can narrow the foramen (the space through which nerve roots exit the spinal cord), potentially compressing nerves — a condition called cervical radiculopathy.
Symptoms may include:
- Radiating pain into shoulders, arms, or hands
- Tingling or numbness
- Muscle weakness
4. Inflammation
Joint inflammation is a common feature of osteoarthritis. Inflammatory mediators released in the neck joints can sensitize nerves and contribute to persistent, dull, or sharp pain.
Who Is at Risk of Cervical Osteoarthritis?
While osteoarthritis is largely age-related, several other factors increase the risk of developing cervical spine OA:
- Age over 50: Natural wear and tear accumulate over time.
- Poor posture: Slouching or forward head posture puts excess stress on cervical joints.
- Repetitive neck strain: Occupations that require prolonged sitting, computer work, or phone usage.
- Previous neck injury: Trauma can accelerate disc degeneration.
- Genetics: Family history of arthritis increases risk.
- Obesity and inactivity: Excess body weight places strain on spinal structures and promotes inflammation.
Common Symptoms of Osteoarthritis in the Neck
Cervical osteoarthritis can range from mild to severe, and symptoms may develop gradually. Common signs include:
- Chronic neck pain (dull, aching, or sharp)
- Stiffness, especially in the morning or after rest
- Reduced range of motion
- Headaches, often starting at the base of the skull
- Grinding or popping sensation during movement (crepitus)
- Pain that worsens with prolonged activity or poor posture
- Radiating symptoms (if nerves are compressed)
Diagnosis of Cervical Osteoarthritis
Accurate diagnosis requires a combination of medical history, physical examination, and imaging:
1. Clinical Evaluation
- Assessment of pain characteristics, posture, and mobility
- Neurological tests for sensation, reflexes, and muscle strength
2. Imaging Studies
- X-rays: Show joint space narrowing, bone spurs, and disc degeneration
- MRI (Magnetic Resonance Imaging): Reveals soft tissue changes, disc health, and nerve compression
- CT scans: Offer detailed images of bone structures
- EMG (Electromyography): May be used to assess nerve function if radiculopathy is suspected
How Is Chronic Neck Pain from Osteoarthritis Managed?
While cervical osteoarthritis is not reversible, symptoms can often be effectively managed through a combination of conservative treatments, lifestyle changes, and physical therapy.
1. Physical Therapy
A tailored physical therapy program focuses on:
- Strengthening neck and upper back muscles
- Improving posture
- Enhancing flexibility and mobility
- Reducing nerve pressure
Manual therapy, traction, and postural re-education are commonly used techniques.
2. Pain Relief Measures
- NSAIDs (e.g., ibuprofen) to reduce inflammation and pain
- Topical analgesics
- Heat and cold therapy for muscle relaxation and inflammation control
- Muscle relaxants for spasms
- Cervical collar (short-term use only) to rest the neck during flare-ups
3. Lifestyle Modifications
- Adjust your workspace ergonomically (monitor at eye level, lumbar support).
- Take frequent breaks if sitting for long periods.
- Sleep with proper neck support (orthopedic pillow).
- Avoid cradling phones between ear and shoulder.
4. Exercise and Movement
Regular movement maintains spinal health and prevents stiffness.
- Gentle stretching: Chin tucks, shoulder rolls, neck side bends
- Low-impact aerobics: Walking, swimming, stationary cycling
- Postural exercises: Wall angels, scapular retractions
Always consult a therapist before starting exercises, especially if symptoms are severe.
5. Advanced Options (If Conservative Measures Fail)
- Injections: Corticosteroid injections can reduce inflammation in affected joints or nerve roots.
- Surgery: Procedures like cervical fusion or disc replacement may be recommended in severe cases with neurological impairment or persistent pain.
Preventing Cervical Osteoarthritis or Delaying Progression
While you can’t completely prevent age-related wear and tear, you can significantly reduce your risk of chronic neck pain from osteoarthritis through:
- Good posture habits
- Regular exercise (particularly strength and mobility work)
- Avoiding prolonged phone or screen use
- Managing body weight
- Staying hydrated (important for disc health)
- Maintaining an anti-inflammatory diet (rich in fruits, vegetables, omega-3s)
When to See a Doctor
See a healthcare provider if:
- Your neck pain lasts more than a few weeks.
- The pain radiates into your arm or hand.
- You experience numbness, tingling, or weakness.
- The pain disrupts your sleep or daily activities.
- Over-the-counter medication is not helping.
Early intervention can prevent complications and improve your quality of life.
Conclusion
Cervical osteoarthritis is a leading cause of chronic neck pain, particularly in older adults. As the neck structures age and degenerate, pain and stiffness can interfere with daily life. Fortunately, by understanding the underlying causes and adopting proactive management strategies, many people can find relief without the need for invasive procedures.
Maintaining neck strength, mobility, and posture — along with timely medical care — is key to minimizing the impact of this degenerative condition and preserving long-term spinal health.
References
- Mayo Clinic. (2021). Preventing back pain. https://www.mayoclinic.org/diseases-conditions/back-pain/in-depth/back-pain/art-20044507
- National Institute of Neurological Disorders and Stroke. (2020). Low back pain fact sheet. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet
- Harvard Health Publishing. (2019). Why good posture matters. Harvard Medical School. https://www.health.harvard.edu/pain/why-good-posture-matters
- World Health Organization. (2019). Musculoskeletal conditions. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions
- National Institutes of Health. (2020). Posture and musculoskeletal health. https://www.ninds.nih.gov/Disorders/All-Disorders/Back-Pain-Information-Page
- Cleveland Clinic. (2021). Cervical spondylosis (arthritis of the neck). https://my.clevelandclinic.org/health/diseases/10155-cervical-spondylosis
- American Physical Therapy Association. (2020). Neck pain. https://www.choosept.com/symptomsconditionsdetail/physical-therapy-guide-to-neck-pain
- Centers for Disease Control and Prevention. (2021). Physical activity for arthritis. https://www.cdc.gov/arthritis/basics/physical-activity-overview.html
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2020). Osteoarthritis. https://www.niams.nih.gov/health-topics/osteoarthritis
- Vos, T., et al. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis. The Lancet. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151183/