Kneecap pain also known as anterior knee pain is a frequent issue that may bother individuals of any age, whether they are an athlete, older adults, or living with a sedentary lifestyle. It generally begins with mild pain which advances slowly to chronic pain unless treatment is initiated. The treatment of kneecap pain must be as early as possible to ensure mobility, prevent long-term injury, and joint health. This blog mentions the causes, diagnosis, the available treatment and preventive measures that can help you to cope with the pain and maintain stronger knees in the long run.
Understanding Kneecap Pain
Definition: What is Kneecap Pain?
Kneecap pain refers to discomfort localized in or around the patella, the small bone at the front of the knee that acts as a protective shield and plays a vital role in leg movement. It is not a single condition but rather a symptom associated with a range of underlying issues, including muscular imbalances, cartilage damage, and inflammatory disorders. The pain can be temporary, linked to overexertion, or persistent, resulting from structural or degenerative problems.
Anatomy of the Kneecap and Its Role in Knee Function
The patella sits within the patellar tendon, connecting the quadriceps muscles in the thigh to the tibia (shinbone) [1]. Its main function is to act as a lever, improving the efficiency of knee extension. The back of the kneecap is covered with articular cartilage, which allows smooth gliding during movement. Surrounding structures such as ligaments, tendons, and synovial fluid provide stability and cushioning. Any damage to these components; whether from injury, overuse, or disease, can disrupt knee mechanics, resulting in pain and reduced mobility.
Types of Kneecap Pain: Acute vs. Chronic
- Acute kneecap pain typically arises from sudden injuries, such as a fall, sprain, or dislocation. The pain is sharp, immediate, and often accompanied by swelling.
- Chronic kneecap pain develops gradually due to repetitive strain, arthritis, or long-term biomechanical imbalances [2]. This type of pain often worsens with activities like climbing stairs, squatting, or sitting for long periods.
Recognizing whether the pain is acute or chronic is essential for choosing the right treatment approach.
Who is Most at Risk?
Certain populations are more susceptible to kneecap pain:
- Athletes: Especially runners, cyclists, and jumpers, who put repeated stress on the patella.
- Older adults: Age-related wear and tear of cartilage increases the risk of osteoarthritis.
- Sedentary individuals: Lack of movement weakens supportive muscles, while prolonged sitting can stiffen the knee joint.
- Overweight individuals: Extra body weight increases pressure on the kneecap, accelerating damage.
Causes of Kneecap Pain
Kneecap pain can stem from multiple factors, ranging from overuse to degenerative conditions. Understanding these causes is critical for effective diagnosis and treatment.
1. Patellofemoral Pain Syndrome (Runner’s Knee)
One of the most frequent causes of kneecap pain, patellofemoral pain syndrome (PFPS), occurs when the patella does not move smoothly in its groove at the end of the femur [3]. It is often linked to repetitive motion, poor alignment, or weak thigh muscles. Runners, dancers, and athletes commonly experience this condition, which worsens during stair climbing, squatting, or sitting with bent knees for prolonged periods.
2. Chondromalacia Patella (Cartilage Softening)
Chondromalacia involves the softening and breakdown of cartilage behind the kneecap. When cartilage wears down, the bone surfaces rub against each other, leading to pain and grinding sensations. This condition is often a progression of PFPS and is particularly common among young adults and athletes [4].
3. Arthritis Affecting the Kneecap
Several forms of arthritis can impact the patella:
- Osteoarthritis: Age-related cartilage degeneration that causes stiffness and chronic pain.
- Rheumatoid arthritis: An autoimmune condition leading to inflammation of the synovial lining.
- Post-traumatic arthritis: Develops after knee injuries that damage cartilage or bone [5].
Arthritis-related kneecap pain usually worsens with age and requires long-term management.
4. Sports Injuries: Sprains, Dislocations, and Fractures
Athletes are particularly vulnerable to acute knee injuries:
- Sprains: Stretching or tearing of ligaments around the kneecap.
- Dislocations: The patella slips out of its groove, causing immediate pain and swelling.
- Fractures: Direct trauma from falls or accidents may fracture the kneecap, requiring surgical intervention.
5. Overuse and Repetitive Strain
Repetitive movements, especially in physically demanding jobs or high-impact sports, can strain the kneecap. Microtrauma from daily wear eventually accumulates, causing chronic inflammation and pain.
6. Obesity and Excess Load on the Knee Joint
Excess weight increases the mechanical load on weight-bearing joints. Every extra kilogram of body weight translates to several additional kilograms of force exerted on the knees during walking or climbing stairs. This accelerates cartilage breakdown and predisposes individuals to arthritis and chronic kneecap pain.
7. Poor Posture, Weak Muscles, or Biomechanical Imbalances
Poor posture, muscle imbalances, or misalignment of the hips and feet can alter patellar tracking. For example:
- Weak quadriceps may fail to stabilize the patella properly.
- Flat feet can change gait mechanics, adding stress to the knee [6].
- Hip muscle weakness can affect knee alignment, leading to pain.
These biomechanical issues often go unnoticed until they result in chronic kneecap discomfort.
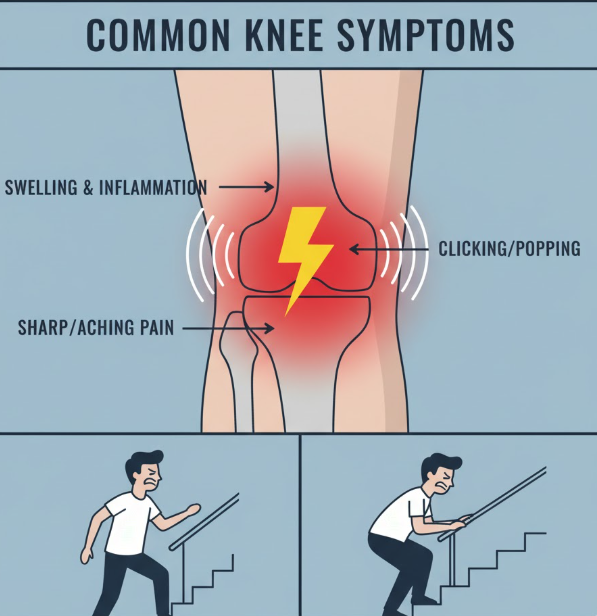
Symptoms of Kneecap Pain
Kneecap pain can present differently depending on the underlying cause, severity, and duration. Recognizing the symptoms early can help in effective diagnosis and treatment.
1. Aching or Sharp Pain Around the Front of the Knee
The most common symptom is pain localized around or behind the kneecap. This discomfort may feel like a dull ache in mild cases or sharp, stabbing pain in severe conditions. Activities such as kneeling, squatting, or standing after long sitting periods often intensify the pain.
2. Swelling, Redness, and Inflammation
Inflammation is the body’s natural response to injury or overuse. The kneecap may appear swollen, tender to the touch, or visibly red. Swelling can restrict knee movement and worsen discomfort during physical activity.
3. Clicking, Popping, or Grinding Sounds
Many individuals report crepitus, a sensation of grinding or crackling when moving the knee. This often indicates cartilage damage or misalignment of the kneecap. Clicking or popping without pain is usually harmless, but when accompanied by discomfort, it requires medical attention.
4. Pain During Climbing Stairs, Squatting, or Sitting Long Hours
Known as the “theater sign” or “moviegoer’s sign,” prolonged sitting with bent knees can lead to stiffness and pain once movement resumes [7]. Similarly, stair climbing or descending places additional pressure on the kneecap, often worsening symptoms.
5. Limited Mobility or Weakness
Severe kneecap pain may cause reduced range of motion, making it difficult to bend, straighten, or bear weight on the knee. Muscle weakness in the quadriceps and surrounding structures often accompanies chronic knee issues, further reducing stability.
Diagnosis of Kneecap Pain
Accurate diagnosis is critical to distinguish between temporary discomfort and underlying medical conditions that require targeted treatment.
Physical Examination and Patient History
The first step involves a clinical assessment by a healthcare provider. They review the patient’s medical history, activity level, and onset of symptoms. Physical examination includes:
- Checking for swelling, tenderness, or deformity.
- Assessing range of motion and flexibility.
- Testing strength in surrounding muscles.
- Evaluating gait and posture.
Imaging Tests
Imaging is often necessary to identify structural problems.
- X-rays: Reveal bone abnormalities, fractures, or alignment issues.
- MRI scans: Provide detailed views of cartilage, ligaments, and tendons. Ideal for detecting soft tissue injuries and cartilage wear.
- CT scans: Offer a more precise evaluation of bone alignment and joint structure.
Laboratory Tests
In cases where infection or arthritis is suspected, blood tests or joint fluid analysis may be performed. These tests help identify autoimmune conditions such as rheumatoid arthritis or detect infections that contribute to joint inflammation.
When to Seek Medical Attention
Mild kneecap pain may resolve with rest, but urgent medical care is necessary if:
- Pain persists beyond a few weeks despite self-care.
- There is sudden, severe swelling.
- The kneecap appears deformed or dislocated.
- Weight-bearing is impossible without significant pain.
Effective Exercises and Movement Practices for Kneecap Pain Relief
Targeted movement plays a vital role in managing and preventing knee discomfort caused by overuse, injury, or poor biomechanics. Understanding kneecap pain causes helps tailor the right activity-based approach for recovery. Gentle, structured movement not only supports kneecap pain treatment but also improves joint alignment, muscle strength, and flexibility.
People experiencing pain under the kneecap while walking or early kneecap injury symptoms often benefit from low-impact, controlled exercises that reduce joint stress. Strength-focused routines such as quadriceps activation, hamstring stretches, and hip-strengthening movements are among the most effective exercises for kneecap pain, as they stabilize the patella and improve tracking during movement.
Mind–body practices like yoga are especially helpful for long-term knee health. Yoga enhances flexibility, balance, and muscle coordination while reducing inflammation and stiffness around the knee joint. Regular practice can improve mobility, reduce chronic pain, and support overall joint resilience when combined with proper medical care and physiotherapy guidance.
Non-Surgical Treatment Options
For most people, kneecap pain can be effectively managed without surgery. Conservative approaches aim to reduce pain, restore mobility, and prevent further damage.
1. Lifestyle Modifications
- Rest and Activity Modification: Reducing activities that aggravate the knee while incorporating gentle movements prevents worsening of symptoms.
- Weight Management: Losing excess body weight reduces stress on the knee joint, lowering the risk of cartilage damage.
- Proper Footwear and Orthotics: Supportive shoes and custom orthotics improve gait alignment, preventing uneven stress on the kneecap.
2. Home Remedies
Simple remedies can bring significant relief:
- RICE Method (Rest, Ice, Compression, Elevation): A classic approach to reduce swelling and pain after acute injury [8].
- Heat Therapy: Helps relax muscles and reduce stiffness, especially for chronic conditions.
- Gentle Stretching: Promotes blood flow and keeps muscles flexible.
3. Physical Therapy and Exercise
Physical therapy is a cornerstone of knee pain management. Therapists design personalized programs to strengthen and stabilize the knee.
- Quadriceps Strengthening: Strong quadriceps muscles support the kneecap and reduce pressure.
- Hamstring and Calf Stretches: Maintain flexibility and reduce strain on the knee joint.
- Low-Impact Exercises: Cycling, swimming, and yoga improve joint function without excessive stress.
- Balance and Stability Training: Prevents falls and improves overall knee mechanics.
4. Supportive Devices
Devices can provide added stability and relief.
- Knee Braces and Straps: Keep the kneecap in proper alignment and reduce pain during activity.
- Orthotic Inserts: These orthotic inserts correct biomechanical imbalances, especially in people with flat feet or misaligned gait.
5. Medications
Medications are often used to control pain and inflammation.
- Over-the-Counter (OTC): NSAIDs such as ibuprofen and acetaminophen relieve mild to moderate pain [9].
- Prescription Drugs: For severe inflammation, doctors may prescribe stronger anti-inflammatory drugs.
- Topical Ointments and Gels: Provide localized pain relief with fewer systemic side effects.
6. Nutrition and Supplements
A healthy diet plays an important role in joint care.
- Anti-Inflammatory Foods: Fatty fish, turmeric, ginger, berries, and leafy greens reduce inflammation.
- Calcium and Vitamin D: Strengthen bones and support cartilage function.
- Joint Supplements: Glucosamine, chondroitin, and collagen are widely used to support cartilage repair and reduce discomfort.
Surgical Treatment Options
When conservative methods fail to provide relief, surgery may become necessary. Surgery is usually recommended for patients with advanced arthritis, severe cartilage damage, or chronic misalignment of the kneecap.
1. Arthroscopy for Repairing Cartilage
Arthroscopy is a minimally invasive surgery where small instruments and a camera are inserted into the knee joint [10]. Surgeons can remove loose cartilage, repair minor tears, and smooth rough surfaces. It allows for quicker recovery compared to open surgery.
2. Realignment Procedures for Patellar Tracking Issues
In some patients, the kneecap does not move smoothly within its groove (patellofemoral maltracking). Realignment surgery repositions tendons and ligaments, ensuring better kneecap stability.
3. Knee Replacement in Severe Arthritis Cases
When arthritis severely damages the knee joint, a partial or total knee replacement may be necessary. Artificial implants replace the worn-out cartilage and bone, relieving pain and restoring mobility.
4. Risks and Recovery Process After Surgery
While surgery can be life-changing, it carries risks such as infection, blood clots, and stiffness. Recovery often involves months of physical therapy to restore function, but long-term outcomes are generally positive if patients adhere to rehabilitation.
Exercises for Kneecap Pain Relief
Exercise remains one of the best tools for both managing and preventing kneecap pain. These exercises strengthen muscles, improve flexibility, and enhance joint stability.
1. Stretching for Flexibility
Gentle stretches for hamstrings, calves, and quadriceps relieve tightness and reduce pressure on the kneecap. Regular stretching improves mobility and reduces stiffness.
2. Strengthening Quadriceps and Hamstrings
The quadriceps muscle plays a key role in supporting the kneecap. Exercises like straight leg raises, wall sits, and step-ups help strengthen these muscles. Strong hamstrings balance the knee joint, preventing instability.
3. Glute and Hip Strengthening for Knee Alignment
Weak hips and glutes can cause improper alignment, increasing kneecap stress. Clamshells, bridges, and side leg lifts strengthen these areas, ensuring better knee mechanics.
4. Low-Impact Aerobic Exercises
Swimming, cycling, and elliptical workouts provide cardiovascular benefits without excessive joint stress. They also help maintain a healthy weight, indirectly easing knee pain.
5. Tips for Safe Exercise Routines
- Warm up before activity.
- Avoid sudden, high-impact movements.
- Progress gradually in intensity.
- Listen to your body and stop if pain worsens.
Preventing Kneecap Pain
Prevention is always better than cure. Small lifestyle changes can significantly reduce the risk of future pain.
1. Maintaining a Healthy Weight
Every extra pound adds stress on the knees. Keeping weight in a healthy range reduces strain and prevents early wear and tear.
2. Proper Warm-Up and Cool-Down During Workouts
Stretching before and after exercise improves flexibility and lowers the chance of injury.
3. Wearing Appropriate Footwear
Shoes with proper cushioning and support prevent misalignment that can worsen knee pain. Athletes should replace worn-out shoes regularly.
4. Avoiding Overtraining and Giving Knees Rest
High-impact activities should be balanced with rest days to prevent overuse injuries.
5. Regular Strength Training to Support Knee Stability
Building strong muscles around the knee ensures stability and long-term joint health.
Psychological and Lifestyle Impact
Living with chronic kneecap pain goes beyond physical discomfort; it can deeply affect emotional health, daily routines, and social participation. Persistent pain often leads to frustration, stress, and reduced motivation, making it harder for individuals to stay active and engaged. Limited mobility can make simple activities, such as climbing stairs, standing for long periods, or walking longer distances, increasingly challenging, which in turn may reduce independence and confidence. To cope with these challenges, mental health support plays an important role. Approaches like cognitive-behavioral therapy (CBT), mindfulness practices, and stress-reduction techniques can help patients better manage the emotional burden of chronic pain [11]. In addition, support groups and community resources provide valuable encouragement, offering a space where individuals can share experiences, learn coping strategies, and feel less isolated in their journey. By addressing both the physical and psychological aspects of kneecap pain, people can improve their overall quality of life and maintain a stronger sense of well-being despite ongoing challenges.
Future Treatments for Kneecap Pain
1. Regenerative Medicine (PRP, Stem Cell Therapy)
These cutting-edge treatments aim to repair damaged cartilage and reduce inflammation naturally.
2. AI-Based Movement Analysis and Injury Prevention
Wearable devices powered by AI can track movement, detect imbalances, and prevent injuries before they happen.
3. Customized Orthotics with 3D Printing
3D-printed orthotics can be tailored to an individual’s unique biomechanics, ensuring better knee support.
4. Advances in Minimally Invasive Surgery
Newer techniques allow faster recovery times, reduced risk, and less post-operative discomfort.
Conclusion
Kneecap pain is quite frequent and may appear to any person, including children and older people. It can be caused by many factors, including injuries, overuse, arthritis and biomechanical issues. Early detection of the symptoms, correct diagnosis and combination of medicine treatment, physical therapy, home care, and lifestyle modification can significantly improve outcomes. Surgery is the last resort in cases where the less invasive procedures have failed. The most effective preventive measures to overcome surgery include losing weight, wearing proper footwear, and exercising.
A comprehensive strategy consisting of physical, nutritional, and mental health care can improve mobility, knee health, and the overall quality of life.
You can experience knee pain for several other reasons. Inserting insoles can help relieve your pain. Know how:
- Custom Insoles for Knee Pain Relief
- How to Choose Insoles Based on Foot Shapes
- Arch Support Insoles for Flat Feet
Frequently Asked Questions:
1. What causes pain under the kneecap?
Pain under the kneecap can result from conditions like patellofemoral pain syndrome, cartilage wear, arthritis, or overuse injuries. Poor alignment or weak muscles can also contribute.
2. How do I know if kneecap pain is serious?
If the pain is severe, lasts for weeks despite rest, or is accompanied by swelling, deformity, or inability to bear weight, it’s time to see a doctor.
3. Can kneecap pain heal without surgery?
Yes. Most cases improve with physical therapy, weight management, supportive devices, and lifestyle adjustments. Surgery is typically the last option.
4. What exercises help strengthen the kneecap?
Quadriceps strengthening (leg raises, wall sits), hamstring stretches, glute bridges, and low-impact activities like cycling and swimming help support knee function.
5. Is running safe if I have kneecap pain?
Running may worsen pain if done excessively or without proper footwear. Switching to low-impact activities and consulting a physiotherapist is recommended before resuming running.
References
- Han, S. W. (2020). Changes in patellofemoral joint mechanics in the presence of quadriceps muscle imbalance.
- Cabrera, A., & Ahn, J. (2025). Knee Pain and Leg Pain. In Musculoskeletal Pain: Evidence-Based Clinical Evaluation and Management (pp. 321-339). Cham: Springer Nature Switzerland. https://doi.org/10.1007/978-3-031-86057-7_14
- Waryasz, G. R., & McDermott, A. Y. (2008). Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dynamic medicine, 7(1), 9. https://doi.org/10.1186/1476-5918-7-9
- Patel, D. R., & Villalobos, A. (2017). Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Translational pediatrics, 6(3), 190. doi: 10.21037/tp.2017.04.05
- Punzi, L., Galozzi, P., Luisetto, R., Favero, M., Ramonda, R., Oliviero, F., & Scanu, A. (2016). Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation. RMD open, 2(2). https://rmdopen.bmj.com/content/2/2/e000279
- Gross, K. D., Felson, D. T., Niu, J., Hunter, D. J., Guermazi, A., Roemer, F. W., … & Hannan, M. T. (2011). Flat feet are associated with knee pain and cartilage damage in older adults. Arthritis care & research, 63(7), 10-1002. doi: 10.1002/acr.20431
- Ophey, M., Frieling, S., Kerkhoffs, G. M., & Tak, I. (2024). Pain during prolonged sitting in subjects with patellofemoral pain in Dutch physical therapy clinics: an online questionnaire-based analysis. BMJ open, 14(11), e086958. https://doi.org/10.1136/bmjopen-2024-086958
- Van Den Bekerom, M. P., Struijs, P. A., Blankevoort, L., Welling, L., Van Dijk, C. N., & Kerkhoffs, G. M. (2012). What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults?. Journal of athletic training, 47(4), 435-443. https://nata.kglmeridian.com/view/journals/attr/attr-overview.xml
- Ruoff, G. M. (2022). OTC analgesics vs opioids for pain management. Journal of Family Practice, 71(6). doi: 10.12788/jfp.0418
- Treuting, R. (2000). Minimally invasive orthopedic surgery: arthroscopy. Ochsner Journal, 2(3), 158-163. https://www.ochsnerjournal.org/content/2/3/158?utm_source=TrendMD&utm_medium=cpc&utm_campaign=Ochsner_Journal_TrendMD_0
- Cherkin, D. C., Sherman, K. J., Balderson, B. H., Cook, A. J., Anderson, M. L., Hawkes, R. J., … & Turner, J. A. (2016). Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. Jama, 315(12), 1240-1249. doi:10.1001/jama.2016.2323