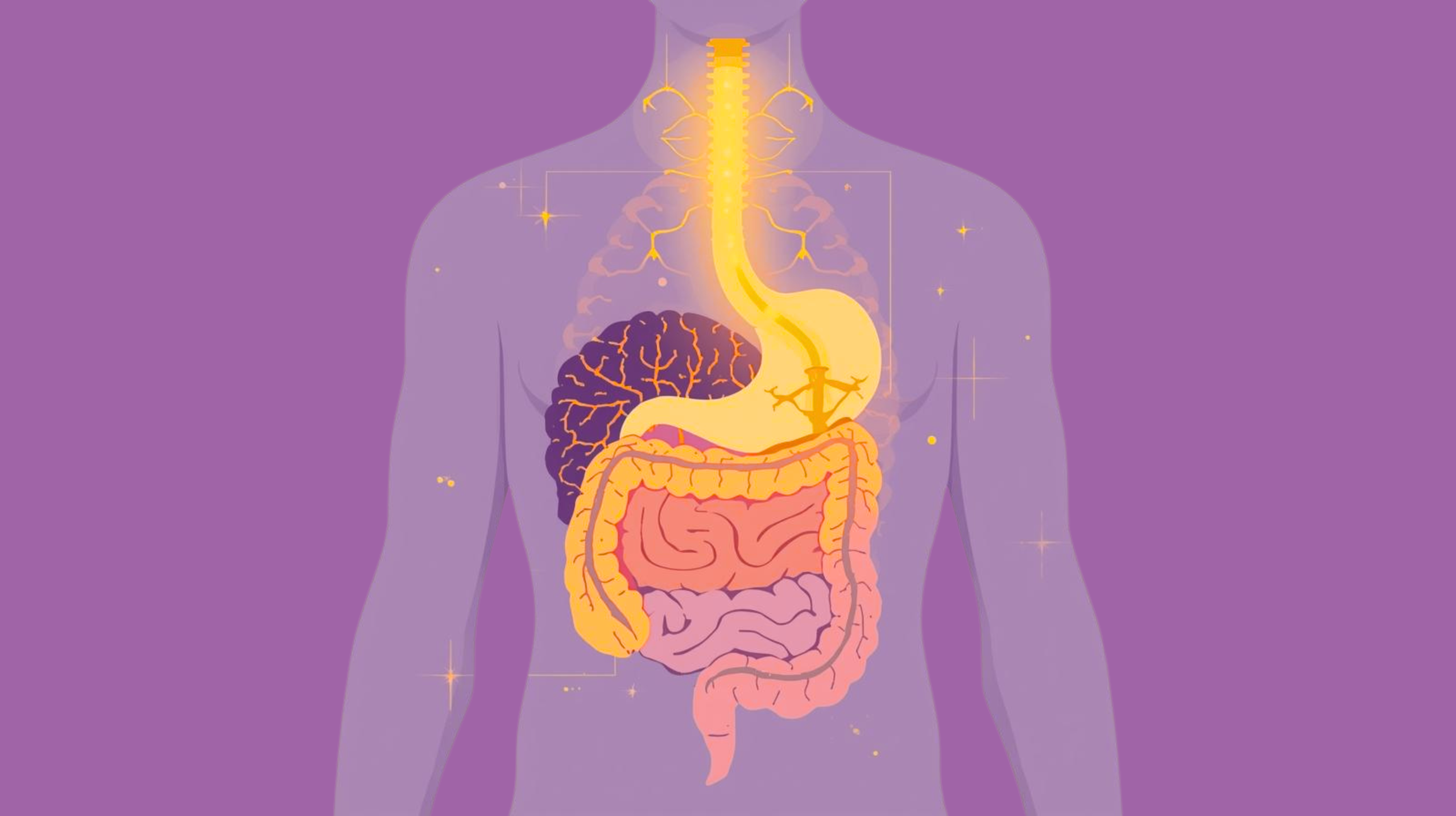
For a long time, mental health has been treated as a problem of thoughts. Change the mindset. Reframe the narrative. Think more positively. But quietly, beneath all that effort, another system has been shaping how you feel long before a single thought appears.
Your gut.
Scientists studying the gut–brain connection made an unexpected observation. People with anxiety, low mood, poor sleep, or constant emotional unease often shared a common factor: chronic gut irritation. Inflammation, food sensitivities, or a compromised gut lining showed up again and again.
Their minds were not failing. Their bodies were signaling distress. And the gut was not subtle about it.
Your Gut Is Not Just Digestive
It Is Emotional. Nearly 90% of your serotonin receptors live in the gut, not the brain. Serotonin doesn’t only influence happiness; it regulates sleep, emotional stability, motivation, and the sense of safety in your body.
When your gut is healthy, serotonin signaling stays balanced. When the gut is inflamed or irritated, that signaling becomes erratic. The brain receives mixed messages and responds by staying alert, cautious, or unsettled.
This is why gut issues rarely show up as stomach problems alone. They show up as mood shifts, restless nights, and emotional fragility that feels hard to explain.
When the Gut Feels Unsafe, So Do You
Leaky gut, chronic inflammation, or repeated exposure to foods your body reacts to allow inflammatory compounds to enter the bloodstream. These compounds can cross into the brain and activate stress pathways.
The result isn’t dramatic panic. It’s something quieter and more persistent.
A sense of unease. Trouble winding down at night. Brain fog after meals. Irritability that feels out of character. Low mood that doesn’t match your life circumstances.
Your brain starts scanning for danger because your body is sending signals that something is wrong.
The Gut–Stress Loop
Once inflammation begins, it often feeds itself. Gut irritation disrupts serotonin production and disrupted serotonin affects sleep and emotional regulation. Poor sleep increases cortisol and stress hormones. Elevated stress further damages digestion and gut lining.
Over time, this creates a loop where emotional stress and gut distress reinforce each other. The problem feels psychological, but the engine driving it is physical.
Everyday Habits That Fuel the Headlines
You don’t need a severe condition for the gut to influence mental health. Small daily habits are enough.
- Eating in a rush while stressed.
- Skipping meals or eating erratically.
- Relying heavily on ultra-processed foods.
- Using caffeine to override fatigue.
- Ignoring bloating, acidity, or discomfort as normal.
Each habit sends a message to the gut that resources are scarce or the environment is unsafe. The gut responds by staying inflamed. The brain responds by staying alert.
The Signs Are Subtle but Consistent
Gut-driven mental health issues often show up as:
- Mood changes linked to meals.
- Feeling emotionally “off” for no clear reason.
- Light anxiety that never fully switches off.
- Sleep that feels unrefreshing.
- Cravings for sugar or comfort foods to feel stable.
These are not personality flaws. They are biological signals asking for support.
Healing Starts With Safety, Not Control
Supporting gut health isn’t about rigid diets or extreme restriction. It’s about restoring a sense of safety in the body.
Eating slowly and choosing foods that feel nourishing rather than stimulating so reducing inflammatory triggers and respecting digestion instead of pushing through discomfort.
When the gut calms down, the nervous system follows. Mood stabilizes not because you forced positivity, but because the body stopped sending distress signals.
The Real Takeaway
Mental health does not begin in the mind alone. It begins in the body systems that decide whether you feel safe enough to rest, connect, and think clearly.
Your gut doesn’t whisper. It writes your emotional headlines daily.
If your mood, sleep, or sense of safety feels fragile, the question may not be what you’re thinking wrong but what your body is struggling to process.
Because sometimes, healing the mind starts by listening below the neck.
Co- authored by: Shayamal Vallabhjee
Chief Science Officer: betterhood
Shayamal is a Human Performance Designer who works at the intersection of psychology, physiology, and human systems design, for the last 25 years he is helping high-performing leaders, teams, and athletes thrive in environments of stress, complexity, and change. His work spans across elite sports, corporate leadership, and chronic health—and is grounded in the belief that true performance isn’t about pushing harder, but designing better.