The human foot is an extraordinary structure designed to provide balance, stability, and mobility. Central to its function is the arch system, which plays a critical role in shock absorption, distributing weight evenly, and supporting posture. However, when the arches collapse, a condition commonly known as flatfoot or fallen arches, the consequences often extend far beyond the feet themselves.
Arch collapse is surprisingly common in modern populations, with estimates suggesting that up to 20–30% of adults experience some form of flatfoot. While many people associate the condition with foot discomfort, its impact on the body is far more profound. The collapse alters biomechanics, triggering a ripple effect on the knees, hips, and spine. Left unaddressed, it can contribute to chronic pain, postural problems, and long-term joint degeneration.
This article explores the anatomy of the foot arch, the mechanics of collapse, the systemic symptoms it causes, associated medical conditions, diagnostic methods, treatment strategies, and emerging innovations in orthotic technology. The thesis is clear: foot arch collapse is not just a localized problem, it affects the entire musculoskeletal chain.
Understanding Foot Arch Anatomy
1. Structure and Function of the Arches
The foot is composed of 26 bones, 33 joints, and over 100 muscles, tendons, and ligaments, all working together to support body weight and provide mobility. Within this structure lie three critical arches:
- Medial longitudinal arch – the highest and most visible arch, running along the inside of the foot. It is primarily responsible for absorbing shock during walking or running.
- Lateral longitudinal arch – located on the outer side of the foot, this arch provides stability.
- Transverse arch – running across the midfoot, this arch helps distribute body weight evenly across the foot.
Together, these arches act like a spring system, maintaining balance and adapting to various surfaces.
2. Types of Arch Collapse
Arch collapse can occur in several forms:
- Flexible flatfoot – The arch appears normal when non-weight-bearing but flattens upon standing. This type is common in children and may persist into adulthood.
- Rigid flatfoot – The arch remains collapsed both in standing and sitting positions. Often more severe, it can result from structural abnormalities or arthritis.
- Progressive arch collapse – Typically occurs with age, injury, or obesity, as ligaments and tendons lose strength and elasticity.
3. Risk Factors for Arch Collapse
Several factors increase the likelihood of developing fallen arches:
- Genetics – Family history of flat feet.
- Obesity – Excess body weight places continuous strain on the arches.
- Diabetes – Alters nerve and tendon function, weakening arch support.
- Ligament laxity – Loose ligaments reduce arch stability.
- Prolonged standing – Occupations requiring long hours on hard surfaces.
- Improper footwear – Shoes without adequate support accelerate arch breakdown.
Biomechanics of Arch Collapse
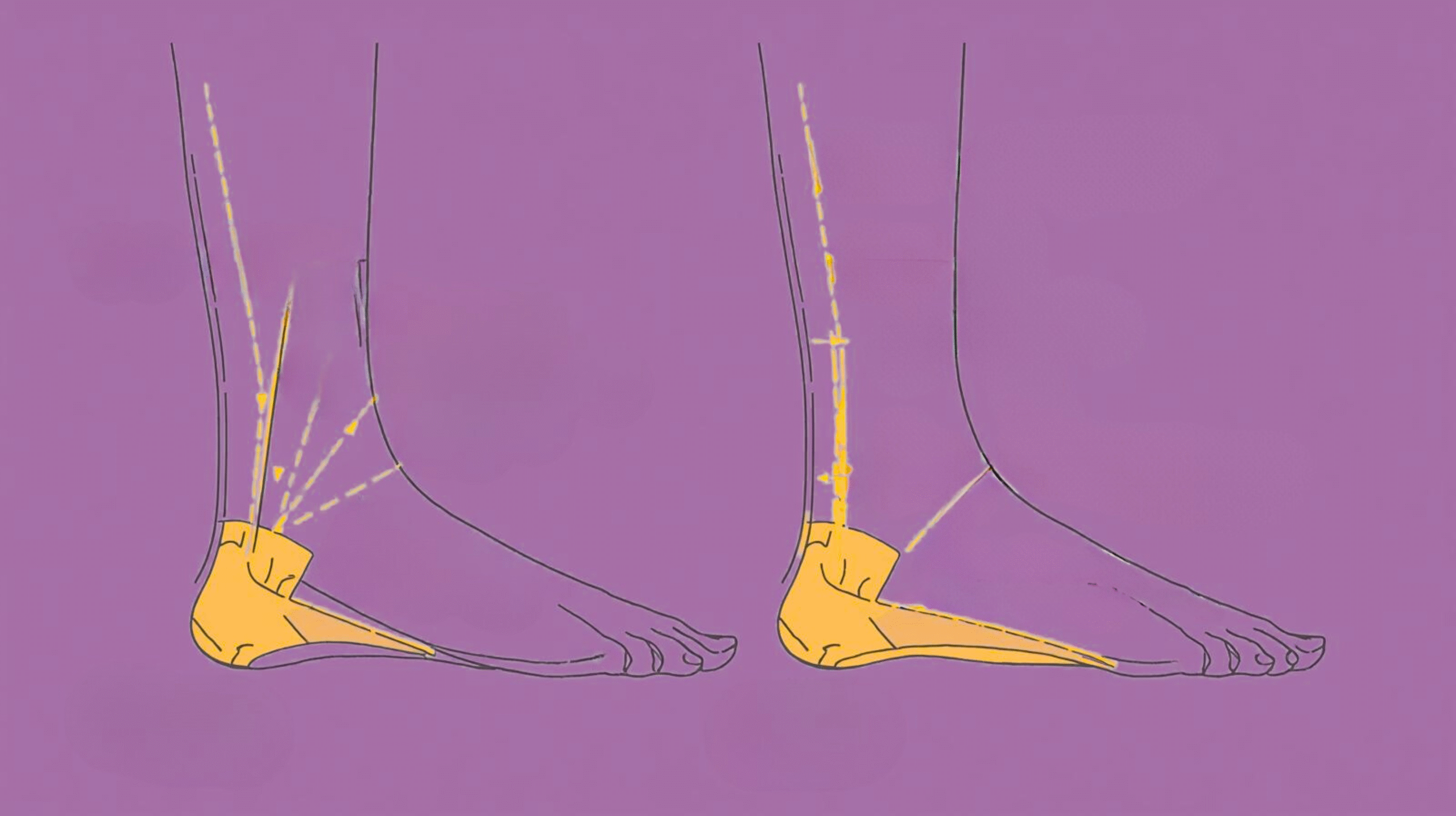
1. Overpronation and Gait Changes
One of the key biomechanical consequences of arch collapse is overpronation, where the foot rolls excessively inward during walking. This disrupts the normal gait cycle and alters the alignment of the ankle and knee. Over time, the abnormal rolling places extra strain on ligaments and tendons, making movement less efficient and more fatiguing.
2. Chain Reaction in the Lower Body
The misalignment caused by fallen arches does not stop at the feet. The effects travel upward:
- At the ankle, instability increases the risk of sprains.
- At the knee, inward rotation stresses the cartilage and ligaments, contributing to pain and early arthritis.
- At the hip, compensatory adjustments strain the muscles responsible for stabilization.
- At the spine, changes in pelvic tilt alter lumbar curvature, resulting in chronic back pain.
3. Altered Shock Absorption
Healthy arches absorb and distribute forces from walking and running. Collapsed arches eliminate this natural cushioning, allowing impact forces to transmit directly into joints. The result is greater wear and tear on the knees, hips, and lower spine.
Symptoms Beyond Foot Pain
1. Knee Problems
Collapsed arches significantly affect knee function. Patellofemoral pain syndrome (PFPS), or “runner’s knee,” often develops when poor foot mechanics disrupt the alignment of the kneecap. Additionally, increased pressure on the inner knee accelerates osteoarthritis, particularly in the medial compartment.
2. Hip Issues
When the foot rolls inward excessively, the femur (thigh bone) rotates inward as well. This disrupts hip mechanics, straining stabilizing muscles such as the gluteus medius. The result can be bursitis or reduced hip mobility, leading to pain with walking or climbing stairs.
3. Lower Back Pain
Arch collapse contributes to pelvic tilt and altered lumbar spine curvature. This biomechanical distortion increases strain on the lower back, often manifesting as chronic lumbar pain or even sciatica.
4. Postural Problems
With collapsed arches, individuals may develop:
- A forward lean due to poor balance.
- Uneven weight distribution, increasing fatigue.
- Decreased athletic performance due to inefficiency in movement.
Medical Conditions Associated with Arch Collapse
1. Plantar Fasciitis
One of the most common complications of flat feet is plantar fasciitis, caused by overstretching of the plantar fascia ligament. This leads to stabbing heel pain, especially during the first steps in the morning.
2. Tendon Dysfunction
The posterior tibial tendon plays a key role in arch support. Dysfunction or tears in this tendon often result in progressive arch collapse, known as posterior tibial tendon dysfunction (PTTD).
3. Sciatica and Nerve Pain
Misalignment in the pelvis caused by fallen arches may contribute to compression of spinal nerves. This can result in sciatica, radiating pain that runs from the lower back down the legs.
4. Long-term Joint Degeneration
Over time, the excess strain caused by collapsed arches accelerates joint degeneration, leading to osteoarthritis in the knees, hips, and spine.
Diagnostic Approaches
1. Physical Examination
Doctors may use visual inspection, palpation, and functional tests such as the foot posture index to evaluate arch height and alignment.
2. Gait Analysis
Advanced tools like motion capture systems and pressure mapping identify abnormal load distribution and gait deviations.
3. Imaging
X-rays can reveal bone alignment, while MRI and ultrasound help assess soft tissue damage such as tendon tears or ligament weakness.
Treatment and Prevention Strategies
1. Orthotics and Insoles
Custom orthotics restore alignment and provide arch support. Unlike over-the-counter (OTC) insoles, which mainly offer cushioning, custom insoles are tailored to individual biomechanics.
2. Strengthening Exercises
Targeted exercises help rebuild arch strength:
- Toe curls to activate intrinsic foot muscles.
- Calf raises to strengthen calf and ankle stability.
- Arch lifts to improve arch height.
- Hip and core strengthening to stabilize the kinetic chain.
3. Lifestyle Modifications
Maintaining a healthy weight reduces stress on the arches. Proper footwear with supportive soles and avoiding prolonged standing on hard surfaces also helps.
4. Medical Interventions
- Physical therapy for strengthening and gait retraining.
- Surgical correction (e.g., tendon repair or osteotomy) in severe, unresponsive cases
Real-World Case Studies
- Runner with Knee Pain – A competitive runner developed chronic knee pain traced to overpronation from flat feet. Custom orthotics corrected the gait, reducing pain and restoring performance.
- Office Worker with Hip and Back Pain – Years of desk work and improper footwear led to hip bursitis and lumbar strain. Diagnosis revealed flatfoot as the underlying cause. Orthotics and posture training provided relief.
- Elderly Patient with Mobility Issues – Progressive arch collapse contributed to balance problems and osteoarthritis. Supportive footwear and physical therapy improved mobility and reduced fall risk.
Future Directions in Arch Support
The future of arch support is increasingly high-tech:
- 3D printing enables ultra-customized orthotics at reduced cost.
Smart insoles provide real-time feedback on gait and pressure distribution - Preventive screening programs for athletes and high-risk workers could detect early signs of arch collapse before serious complications arise
Conclusion
Foot arch collapse is far more than a cosmetic or localized issue, it is a biomechanical problem with systemic consequences. From knee and hip pain to chronic lower back problems, the ripple effects of fallen arches highlight the importance of proper diagnosis and treatment.
Early intervention with orthotics, strengthening, lifestyle modifications, and, in severe cases, medical treatment can significantly reduce pain and prevent long-term complications. As technology advances, new solutions promise even more effective prevention and correction.
Bottom line: Treating arch collapse is not just about saving your feet, it’s about protecting your entire musculoskeletal health.
People are also reading:
- How Custom Insoles Can Help Prevent Knee and Hip Pain
- Ergonomic Hacks for Frequent Ride-Share Drivers
- Science of Vibration and Back Pain in Vehicles
- How Seat Angle Affects Your Spine on Long Drives
- Can Your Sitting Posture Cause Hip Misalignment
- Adjustable vs Fixed Car Backrests
Frequently Asked Questions:
1. What are the main causes of foot arch collapse?
Genetics, obesity, diabetes, tendon injuries, prolonged standing, and improper footwear are the most common causes
2. How does flatfoot affect the knees and hips?
Flatfoot causes overpronation, leading to inward knee rotation and hip misalignment. This increases stress on joints, contributing to pain and arthritis.
3. Can collapsed arches cause lower back pain?
Yes. Arch collapse alters pelvic tilt and lumbar spine curvature, which can cause chronic back pain and even sciatica.
4. Is arch collapse reversible with exercise?
In children and mild cases, strengthening exercises may restore arch support. In adults, exercises help manage symptoms but may not fully reverse collapse.
5. Are custom orthotics necessary for treating arch collapse?
Custom orthotics are highly recommended because they correct alignment, reduce pain, and prevent progression, unlike generic insoles.
References:
- Collins, N. J., Bisset, L. M., Crossley, K. M., & Vicenzino, B. (2009). Efficacy of foot orthoses in the treatment of patellofemoral pain syndrome: A randomized clinical trial. BMJ, 338, b1735. https://doi.org/10.1136/bmj.b1735
- Hintermann, B., Nigg, B. M., Sommer, C., & Cole, G. K. (1994). Transfer of movement between calcaneus and tibia in vitro. Clinical Biomechanics, 9(6), 349–355. https://doi.org/10.1016/0268-0033(94)90064-7
- Kulig, K., Reischl, S. F., Pomrantz, A. B., Burnfield, J. M., Mais-Requejo, S., Thordarson, D. B., & Smith, R. W. (2009). Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: A randomized controlled trial. Physical Therapy, 89(1), 26–37. https://doi.org/10.2522/ptj.20070194
- Menz, H. B., Dufour, A. B., Riskowski, J. L., Hillstrom, H. J., & Hannan, M. T. (2013). Foot posture, foot function and low back pain: The Framingham Foot Study. Rheumatology, 52(12), 2275–2282. https://doi.org/10.1093/rheumatology/ket275
- Tiberio, D. (1987). The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. Journal of Orthopaedic & Sports Physical Therapy, 9(4), 160–165. https://doi.org/10.2519/jospt.1987.9.4.160