Pain that does not resolve on its own is termed as chronic pain. The sickness lasts for weeks, months or even years, which is even longer than the recommended time to recuperate. Acute pain signifies an injury or a disease. Chronic pain, on the other hand, may occur without any noticeable cause or persist even after the initial cause.
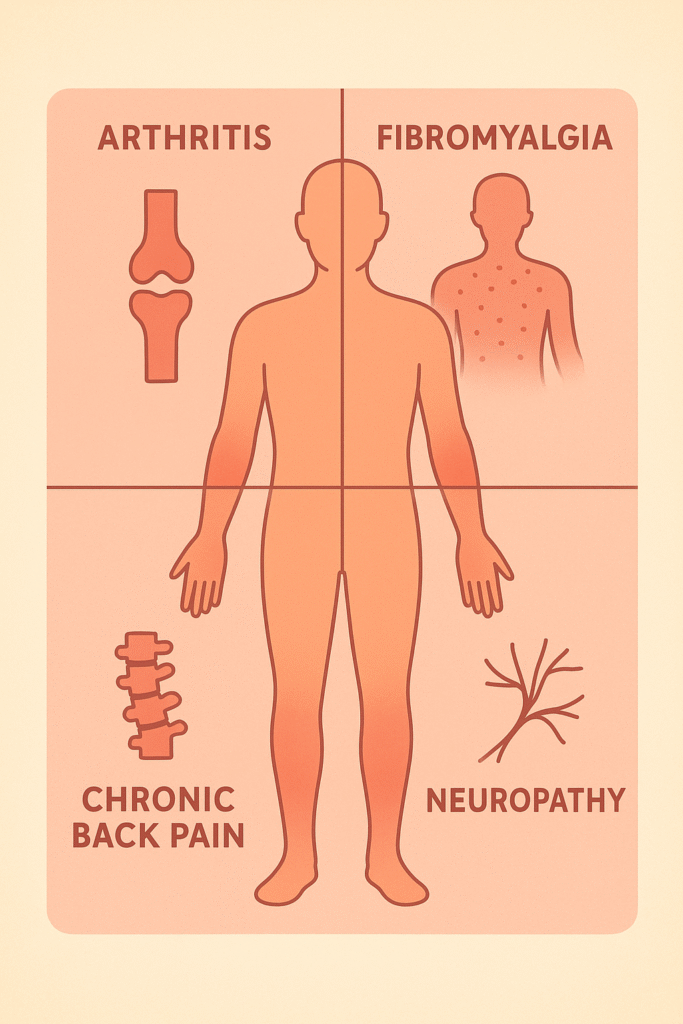
Chronic pain has an immense burden. It negatively impactsyour general standard of living, your capacity to work as well as your body and physical health. Illnesses such as neuropathy, fibromyalgia, arthritis, and back pain impact millions of individuals in the world and complicate their mobility and their ability to perform their activities.
Managing chronic pain is highly important if you want to improve life quality and gain back freedom of moving about. By integrating medical therapy, lifestyle modification and alternative therapy, people are able to gain control over their pains and not the other way round.
Causes and Types of Chronic Pain
Chronic pain arises from various health conditions, each with unique triggers and symptoms.
Common Causes
- Arthritis: A degenerative joint disease leading to stiffness, inflammation, and long-term discomfort.
- Fibromyalgia: A condition marked by widespread muscle pain, fatigue, and tenderness [1].
- Chronic back pain: Often caused by spinal issues, poor posture, or previous injury.
- Neuropathy: Nerve damage leading to tingling, burning, or shooting pains, commonly seen in diabetes.
Types of Pain
- Neuropathic pain: Caused by nerve damage, producing sensations like burning, stabbing, or electric shocks.
- Nociceptive pain: Results from tissue damage or inflammation, such as arthritis or injury-related pain [2].
Impact on Daily Life
Chronic pain can severely reduce mobility, making simple tasks like walking, cooking, or even sleeping difficult. Over time, it contributes to frustration, depression, anxiety, and feelings of helplessness, underscoring the need for comprehensive pain management.
Understanding the Impact of Chronic Pain
The effects of chronic pain extend far beyond the body.
- Physical limitations: Restricted mobility, muscle weakness, and fatigue can make routine activities exhausting.
- Emotional and psychological effects: Constant discomfort often leads to stress, depression, and anxiety [3]. Pain may even alter brain chemistry, intensifying emotional struggles.
- Economic and social implications: Frequent medical visits, treatment costs, and lost workdays place financial strain on individuals and families. Social isolation is also common, as pain limits participation in activities.
Thus, chronic pain is not only a medical issue but also a biopsychosocial challenge requiring holistic management.
Conventional Medical Treatments
Medical treatments are often the first line of defense in chronic pain management.
Over-the-Counter Pain Relievers
- NSAIDs (e.g., ibuprofen, naproxen): Reduces inflammation and pain but may cause stomach irritation with long-term use.
- Acetaminophen: Provides pain relief without anti-inflammatory effects, safer for the stomach but risky in high doses for the liver [4].
Prescription Medications
- Opioids: Effective for short-term relief but carry high risks of dependency and side effects.
- Muscle relaxants: Relieve spasms associated with back pain or injuries.
- Antidepressants and anticonvulsants: Sometimes used to treat neuropathic pain.
Interventional Procedures
- Injections: Corticosteroid or anesthetic injections for joint or spinal pain.
- Nerve blocks: Temporarily disrupt nerve signals transmitting pain.
- Surgery: Used as a last resort for severe cases such as herniated discs or joint replacement.
Benefits and Risks
While medical interventions can provide immediate relief, they often address symptoms rather than root causes. Long-term reliance on medications can lead to side effects, making it crucial to balance medical care with lifestyle and holistic strategies.
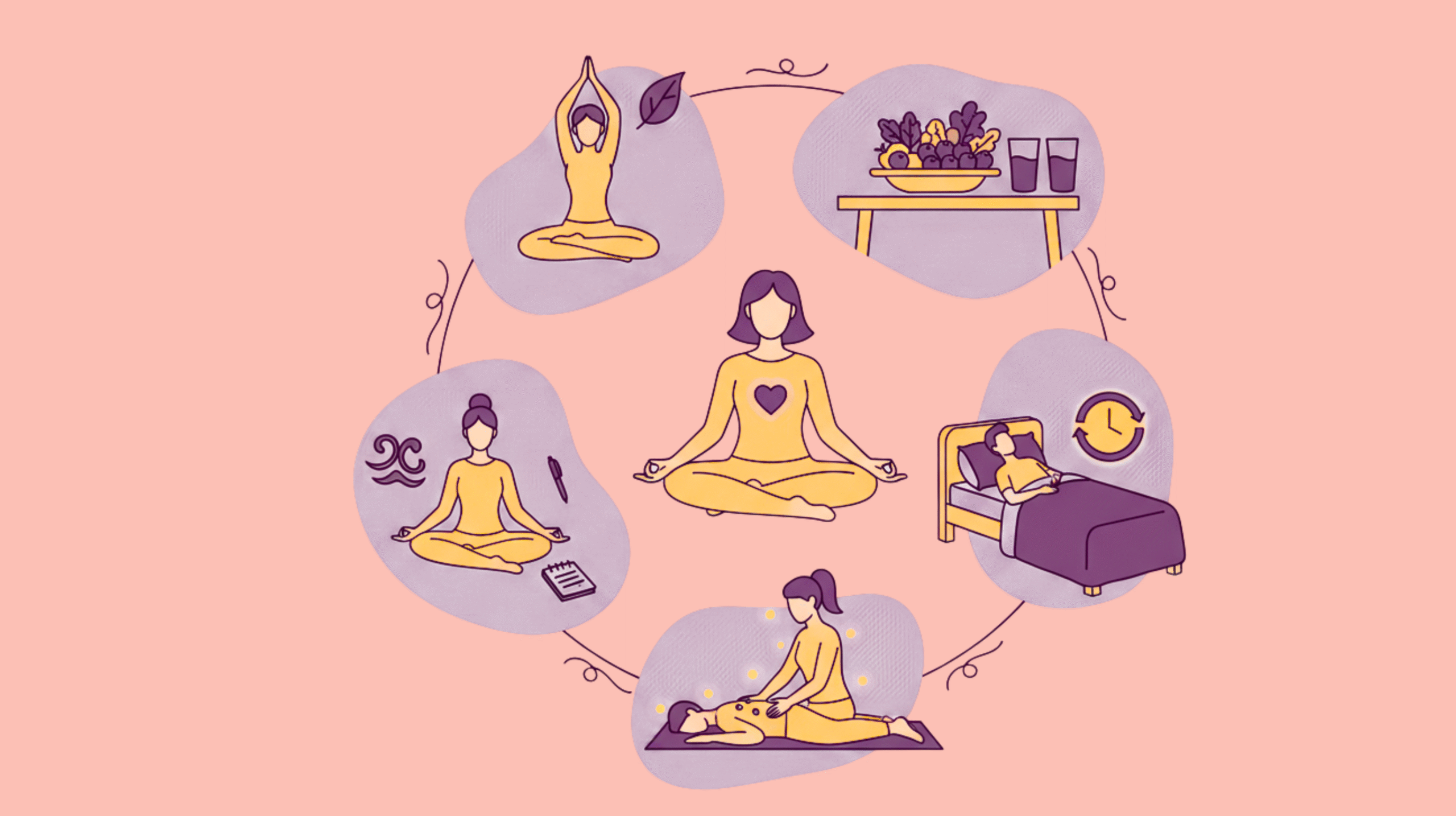
Lifestyle Strategies for Chronic Pain Relief
Lifestyle modifications form the backbone of sustainable pain management.
1. Exercise and Physical Therapy
- Low-impact exercises: Swimming, yoga, or walking improve mobility without stressing joints.
- Strength and flexibility training: Enhances muscle support around painful joints.
- Physical therapy: Tailored programs guided by professionals to restore function and reduce pain.
2. Nutrition and Anti-Inflammatory Diet
- Foods that reduce inflammation: Berries, fatty fish, nuts, olive oil, and leafy greens [5].
- Avoiding pro-inflammatory foods: Sugary drinks, processed snacks, and trans fats.
- Hydration: Adequate water intake reduces joint stiffness and improves overall recovery.
3. Sleep and Rest
- Chronic pain disrupts sleep cycles, worsening symptoms.
- Sleep hygiene tips: Maintain a consistent bedtime, limit screen use before bed, and create a calm environment.
- Restorative sleep is crucial as the body heals and regulates pain perception during deep sleep phases.
4. Stress Management and Mental Health
- Cognitive-behavioral therapy (CBT): Helps reframe negative thoughts about pain [6].
- Mindfulness and meditation: Promote relaxation and reduce the perception of pain.
- Stress reduction techniques: Breathing exercises, journaling, or engaging in hobbies.
5. Alternative and Complementary Therapies
- Acupuncture and acupressure: Stimulate pressure points, improving circulation and reducing pain signals.
- Massage therapy and myofascial release: Alleviate tension and improve flexibility.
- Heat and cold therapy: Ice reduces inflammation, while heat relaxes stiff muscles.
- Chiropractic care: Helps realign the spine and relieve back or neck pain.
Medications vs. Natural Remedies: Pros and Cons
When it comes to chronic pain, patients and healthcare providers often face a key decision: Should pain be managed primarily through medications, or should natural remedies and lifestyle-based approaches be prioritized? In practice, the most effective strategies usually involve a balance of both.
When to Use Medications?
Medications are especially helpful during flare-ups of pain that are intense and disruptive. For instance, NSAIDs (ibuprofen, naproxen) can quickly reduce inflammation in arthritis, while anticonvulsants or antidepressants may provide relief for neuropathic pain [7]. In more severe cases, opioids are prescribed, though they are ideally used short-term due to their addictive potential. Medications offer fast relief and allow patients to maintain functionality when pain peaks.
Risks of Long-Term Drug Use
Over-reliance on medications carries risks. Long-term NSAID use can cause gastrointestinal bleeding or kidney problems, while opioids bring the danger of tolerance, dependency, and overdose. Even seemingly “safe” over-the-counter drugs like acetaminophen can cause liver damage in high doses. For this reason, most experts recommend medications as one part of a broader plan, rather than a sole strategy.
Natural Remedies and Their Benefits
Natural remedies emphasize prevention and long-term management. Anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and whole foods can reduce inflammation and stiffness. Herbal remedies like turmeric and ginger have been studied for their analgesic effects [8]. Techniques like yoga, meditation, and acupuncture not only alleviate pain but also improve mental resilience. Unlike medications, these methods support overall health without significant side effects when practiced correctly.
Integrating Both Approaches
The strongest results usually come from integration. For example, someone with arthritis may take NSAIDs during a flare-up while following an anti-inflammatory diet, practicing yoga, and receiving massage therapy regularly. This reduces dependency on drugs while still providing relief when pain becomes unmanageable.
In short: Medications provide quick relief, but natural remedies offer long-term resilience. Balancing the two prevents over-reliance on drugs while empowering patients with lifestyle-based control over their condition.
Creating a Personalized Chronic Pain Management Plan
No two cases of chronic pain are identical. For effective management, it’s essential to create a plan tailored to an individual’s condition, lifestyle, and goals.
Assessing Pain and Triggers
The first step is identifying the root causes and aggravating factors. Some patients may experience pain primarily due to inflammation, while others struggle with neuropathy or muscle tightness. Journaling pain levels, diet, activity, and stress can help uncover patterns. For instance, a patient may notice that certain foods or poor sleep worsen their symptoms.
Balancing Medical Treatments and Lifestyle Adjustments
A well-designed plan blends conventional medicine with lifestyle changes. Medications may address acute pain, while regular exercise, stretching, and therapy prevent future flare-ups [9]. Nutrition also plays a key role, ensuring the body has the resources to fight inflammation and heal tissues.
Including Alternative Therapies
Complementary approaches such as acupuncture, massage therapy, or chiropractic adjustments can be integrated. These therapies may not replace medication, but they enhance recovery, mobility, and relaxation when used consistently.
Monitoring and Adjusting Over Time
Chronic pain is dynamic; it changes with age, health status, and lifestyle. A personalized plan should be flexible, regularly reviewed with healthcare providers, and adjusted based on progress. For example, a patient who improves mobility through physiotherapy may reduce reliance on medications and increase focus on exercise and diet.
Empowerment and Self-Management
An often-overlooked aspect of chronic pain management is empowerment. Patients who feel in control of their routines, track progress, set goals, and engage in active coping strategies report better outcomes than those relying passively on medication.
Key takeaway: A personalized plan is not static but evolves over time. It combines medical interventions, lifestyle practices, and alternative therapies with active monitoring to ensure long-term relief and quality of life.
Common Mistakes in Chronic Pain Management
Even with good intentions, many people make mistakes that worsen chronic pain or slow recovery. Avoiding these pitfalls is as important as following a treatment plan.
1. Ignoring Pain Signals
Some individuals push through pain, believing endurance will make them stronger. While mild discomfort during physical therapy can be normal, ignoring severe pain risks injury, worsened inflammation, and delayed recovery. Listening to the body is crucial.
2. Over-Reliance on Medications
Medications can mask pain but do not address its underlying causes. Relying solely on drugs may allow inflammation or poor posture to worsen unnoticed [10]. Moreover, long-term use carries significant risks, making it dangerous to depend only on pharmaceutical relief.
3. Sedentary Lifestyle
Many people with chronic pain avoid movement out of fear of worsening symptoms. However, immobility weakens muscles, reduces flexibility, and can actually amplify pain. Gentle exercise and physical therapy are vital for breaking this cycle.
4. Poor Sleep Hygiene
Sleep is often neglected, but lack of quality rest amplifies pain sensitivity. Skipping consistent bedtimes, using screens late at night, or consuming caffeine before bed can sabotage recovery. Sleep hygiene should be a cornerstone of pain management.
5. Neglecting Nutrition and Hydration
Skipping meals, consuming processed foods, or failing to hydrate can increase inflammation and stiffness. Patients often underestimate the role of diet in pain relief, but an anti-inflammatory diet is as powerful as some medical interventions.
6. Ignoring Mental Health
Chronic pain and mental health are closely linked. Depression, anxiety, and stress intensify the perception of pain. Failing to seek mental health support through therapy, mindfulness, or support groups leaves an important part of the problem unaddressed.
7. Lack of Professional Guidance
Self-managing pain without consulting professionals may lead to harmful practices or missed diagnoses. Regular check-ins with doctors, physiotherapists, or dietitians ensure strategies remain safe and effective.
Conclusion
Stressful pain and suffering that continue to disrupt your physical, mental, and social health are called chronic pain. Effective management requires the use of a multimodal approach that includes medical therapy, alternative medicine, physical activity, nutrition, sleep, and proper mental health. Individuals can completely improve their lives when employing personalized plans and preventing common mistakes. This is not neccesarily eliminating pain, but knowing how to handle it successfully, to be independent again and also live to your fullest despite life challenges.
To be specific, different chronic pain has different relief methods. Check these to know more:
Frequently Asked Questions:
1. What are the most effective strategies for chronic pain relief?
A combination of medical treatments, exercise, nutrition, stress management, and alternative therapies is most effective. Integrating these approaches ensures long-term results.
2. Can exercise help reduce chronic pain?
Yes. Low-impact exercises like swimming, yoga, or walking improve mobility, reduce stiffness, and enhance mood, thereby relieving pain.
3. Which foods are beneficial for managing chronic pain?
Foods rich in anti-inflammatory compounds, such as berries, salmon, leafy greens, nuts, and olive oil, are beneficial, while processed and sugary foods should be avoided.
4. How does sleep affect chronic pain?
Poor sleep intensifies pain perception and fatigue. Good sleep hygiene and restorative sleep significantly reduce symptoms and improve resilience.
5. Are alternative therapies like acupuncture effective for chronic pain?
Yes. Many studies show that acupuncture, massage therapy, and mindfulness can reduce pain levels and improve mental well-being, especially when combined with conventional treatments.
References
- Clauw, D. J. (2015, May). Fibromyalgia and related conditions. In Mayo clinic proceedings (Vol. 90, No. 5, pp. 680-692). Elsevier. https://doi.org/10.1016/j.mayocp.2015.03.014
- Singh, B. M., Negi, G., Bhole, P., & Jaiprakash, M. (2012). Pain and inflammation: a review. International Journal of Pharmaceutical Sciences and Research, 3(12), 4697. https://www.researchgate.net/profile/Brij-Mohan-Singh-3/publication/394937222_PAIN_AND_INFLAMMATION_A_REVIEW/links/68acb037ca495d76982fe180/PAIN-AND-INFLAMMATION-A-REVIEW.pdf
- Ellis, A. (1980). Discomfort anxiety: A new cognitive behavioral construct. Rational living, 15(1), 25-30. https://albertellis.org/wp-content/uploads/2021/09/Discomfort-Anxiety-A-New-Cognitive-Behavioral-Construct-1.pdf
- Alchin, J., Dhar, A., Siddiqui, K., & Christo, P. J. (2022). Why paracetamol (acetaminophen) is a suitable first choice for treating mild to moderate acute pain in adults with liver, kidney or cardiovascular disease, gastrointestinal disorders, asthma, or who are older. Current medical research and opinion, 38(5), 811-825. https://doi.org/10.1080/03007995.2022.2049551
- Galland, L. (2010). Diet and inflammation. Nutrition in Clinical Practice, 25(6), 634-640. https://doi.org/10.1177/0884533610385703
- Broderick, J. E., Keefe, F. J., Schneider, S., Junghaenel, D. U., Bruckenthal, P., Schwartz, J. E., … & Gould, E. (2016). Cognitive behavioral therapy for chronic pain is effective, but for whom?. Pain, 157(9), 2115-2123. DOI: 10.1097/j.pain.0000000000000626
- Zobdeh, F., Eremenko, I. I., Akan, M. A., Tarasov, V. V., Chubarev, V. N., Schiöth, H. B., & Mwinyi, J. (2022). Pharmacogenetics and pain treatment with a focus on non-steroidal anti-inflammatory drugs (NSAIDs) and antidepressants: a systematic review. Pharmaceutics, 14(6), 1190. https://doi.org/10.3390/pharmaceutics14061190
- Terry, R., Posadzki, P., Watson, L. K., & Ernst, E. (2011). The use of ginger (Zingiber officinale) for the treatment of pain: a systematic review of clinical trials. Pain medicine, 12(12), 1808-1818. https://doi.org/10.1111/j.1526-4637.2011.01261.x
- Bowden, J. L., Kobayashi, S., Hunter, D. J., Mills, K., Peat, G., Guillemin, F., … & Eyles, J. P. (2021, August). Best-practice clinical management of flares in people with osteoarthritis: a scoping review of behavioral, lifestyle and adjunctive treatments. In Seminars in arthritis and rheumatism (Vol. 51, No. 4, pp. 749-760). WB Saunders. https://doi.org/10.1016/j.semarthrit.2021.04.017
- Abdallah, Y. E. H., Chahal, S., Jamali, F., & Mahmoud, S. H. (2023). Drug-disease interaction: clinical consequences of inflammation on drugs action and disposition. Journal of Pharmacy & Pharmaceutical Sciences, 26, 11137. https://doi.org/10.3389/jpps.2023.11137