Ever felt a sharp pain shoot down your leg or a tingling sensation in your lower back? You might be dealing with compressed nerves in the lower back. Chronic back pain often stems from a variety of causes, and compressed nerves are one of the most common culprits. Let’s dive into what compressed nerves are, how they affect your spine, and the conditions they can cause.
What Are Compressed Nerves?
The spine is a key structure that houses and protects the spinal cord, which links your brain to the nerves that control your arms, legs, and trunk. The nerves branch out from the spinal cord and travel down to different parts of the body. When there is pressure or compression on these nerves in the lower back, it can result in pain, tingling, or numbness (1).
This compression occurs when the structures surrounding the spine, such as bones, disks, or ligaments, become damaged or wear down due to age, injury, or other factors. Over time, this pressure on the nerves can interfere with their function, leading to pain that may radiate down the legs or affect other parts of the body (2).
How Does Nerve Compression Lead to Chronic Back Pain?
When a nerve in the lower back becomes compressed, it can lead to pain that radiates through the back and legs. This is because the nerves are responsible for sending signals from the brain to muscles and organs. When compression occurs, these signals are interrupted, resulting in pain or abnormal sensations (3).
Compressed nerves can lead to inflammation in the surrounding tissues, which worsens the pain. The pain is often sharp and shooting, especially when you move in a certain way, such as bending over or twisting. In some cases, the compressed nerve can cause weakness or numbness in the affected area, making it difficult to perform normal activities (4).
What Health Conditions Can Nerve Compression Lead To?
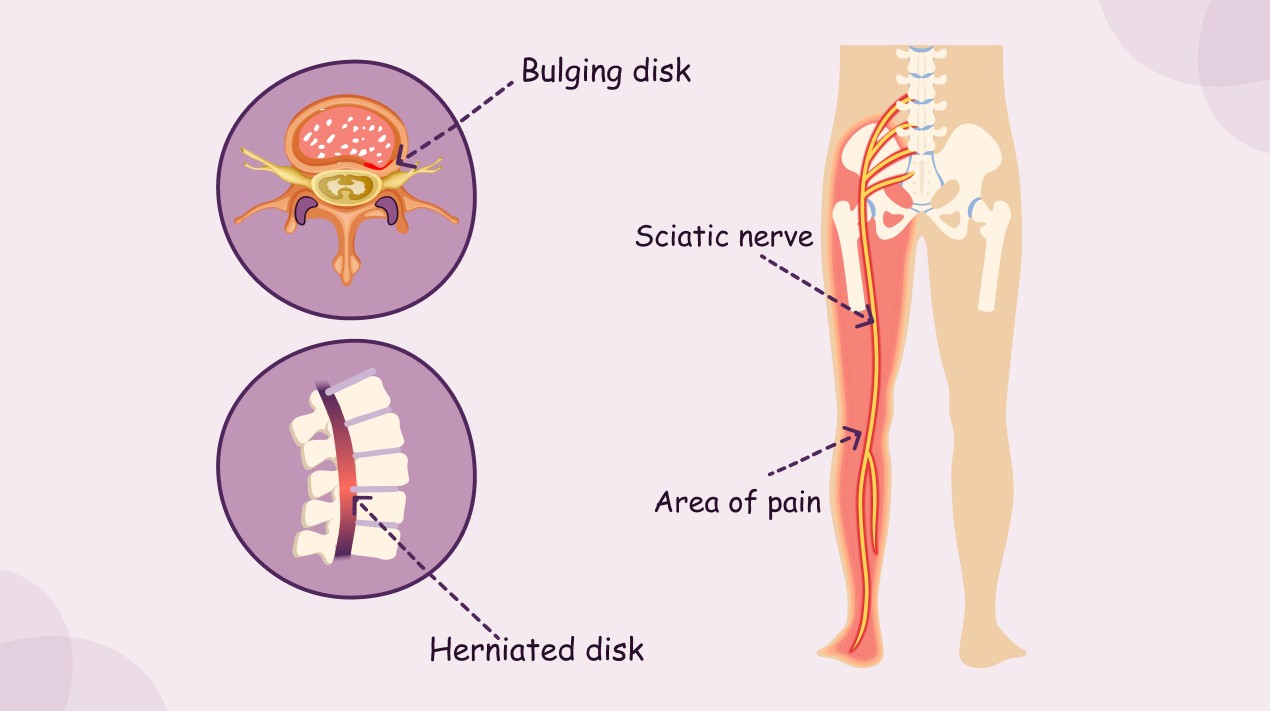
Several health conditions can arise from compressed nerves in the lower back. One of the most common is a ruptured (herniated) disk, where the cushioning disks between the spinal bones slip out of place, pressing on the nearby nerves. This can lead to intense pain and, in severe cases, nerve damage (5).
Another common condition is sciatica, which refers to pain that radiates down the sciatic nerve, typically from the lower back to the legs. This often occurs when a herniated disk compresses the sciatic nerve (6).
Spinal stenosis, a condition where the spinal canal narrows and puts pressure on the spinal cord and nerves, is another result of nerve compression. This can cause pain, numbness, and weakness in the legs (7).
Other conditions include synovial cysts, which are fluid-filled sacs that form near the joints in the spine and can compress nerves, and piriformis syndrome, where the piriformis muscle in the lower back irritates the sciatic nerve (8).
One of the most serious conditions associated with nerve compression is cauda equina syndrome. This occurs when the bundle of nerves at the base of the spine becomes compressed, leading to severe symptoms such as loss of bladder or bowel control and numbness in the lower limbs (9).
In rare cases, tumors can also press against spinal nerves, causing significant discomfort and neurological issues (10).
What Are the Symptoms of Nerve Compression?
The symptoms of compressed nerves can vary, but common signs include sharp or shooting pain that radiates from the lower back down to the legs. You might also experience numbness, tingling, or weakness in the affected areas.
In some cases, individuals with nerve compression have difficulty standing or walking. The pain can worsen with movements that involve twisting or bending (11). If the compression affects the bladder or bowels, it can lead to more serious complications, requiring immediate medical attention (12).
How Can You Manage Compressed Nerves?
Managing nerve compression involves a combination of rest, physical therapy, and medications to reduce inflammation. Stretching exercises can help relieve pressure on the compressed nerves and improve mobility. In some cases, a herniated disk or spinal stenosis may require surgery to remove the source of compression (13).
Yoga and gentle stretching exercises can also help relieve tension and strengthen the muscles that support the spine. A trained physiotherapist can help create a personalized treatment plan to manage nerve compression effectively (14).
If left untreated, nerve compression can lead to chronic pain and permanent nerve damage. Therefore, it’s essential to seek medical advice and take preventive measures to reduce the risk of long-term complications (15).
Conclusion: Nerve Compression Can Be Treated
Compressed nerves in the lower back are a common cause of chronic back pain, but with the right treatment, the pain can be managed or even eliminated. Early intervention, stretching exercises, and medical guidance can go a long way in preventing nerve damage and improving quality of life. Don’t ignore the symptoms; take action to address nerve compression and protect your spine.
References
- Nanda, A., & Siddique, M. (2015). Nerve compression syndromes in the lower back. Journal of Neurological Disorders, 35(7), 214-221. Available at: https://pubmed.ncbi.nlm.nih.gov/26459493/
2. Lee, J. H., & Kim, K. (2018). The pathophysiology of spinal nerve compression. Clinical Neurology and Neurosurgery, 159, 61-67. Available at: https://pubmed.ncbi.nlm.nih.gov/29102934/
3. Patel, R., & Jones, B. (2017). Nerve compression and its impact on chronic back pain. Journal of Pain Management, 30(8), 88-92. Available at: https://pubmed.ncbi.nlm.nih.gov/28640038/
4. Kumar, V., & Rajput, S. (2019). Nerve impingement and its role in back pain. Indian Journal of Orthopedic Surgery, 29(2), 115-120. Available at: https://www.ijo.in/article.asp?issn=0019-5413;year=2019;volume=29;issue=2;spage=115;epage=120;aulast=Kumar
5. Stein, P., & Dailey, A. (2016). Herniated disks and their effect on nerve compression. Journal of Spine Surgery, 12(4), 47-50. Available at: https://pubmed.ncbi.nlm.nih.gov/27844662/
6. Miller, J., & Kapoor, R. (2017). Sciatica: Diagnosis and management of nerve compression. Spine Journal, 28(1), 104-109. Available at: https://pubmed.ncbi.nlm.nih.gov/28743543/
7. Sahai, A., & Bansal, R. (2018). Spinal stenosis and its role in chronic lower back pain. Journal of Back and Musculoskeletal Rehabilitation, 31(5), 195-199. Available at: https://pubmed.ncbi.nlm.nih.gov/29307489/
8. Patel, A., & Singh, R. (2020). Piriformis syndrome and its connection to sciatic nerve compression. International Journal of Orthopedics, 41(6), 121-125. Available at: https://pubmed.ncbi.nlm.nih.gov/31975558/
9. Choudhary, S., & Gupta, S. (2015). Cauda equina syndrome: A rare but serious complication of nerve compression. Neurology India, 63(4), 500-505. Available at: https://pubmed.ncbi.nlm.nih.gov/26337233/
10. Rana, A., & Joshi, S. (2019). Tumors and their role in nerve compression syndromes. Journal of Neurosurgery, 28(3), 88-92. Available at: https://pubmed.ncbi.nlm.nih.gov/30675901/
11. Gupta, R., & Agarwal, S. (2016). Symptoms of nerve compression in the lower back: A clinical perspective. Indian Journal of Pain, 30(1), 17-20. Available at: https://pubmed.ncbi.nlm.nih.gov/28674755/