Knee pain is a common issue that affects people as they age, and one of the primary causes is osteoarthritis (OA). This wear-and-tear condition can lead to pain, stiffness, and a reduced range of motion in the knee joint, making everyday activities increasingly difficult. In this blog, we will explore what osteoarthritis in the knee is, its underlying causes, associated health conditions, and treatment options.
What is Osteoarthritis in the Knee?
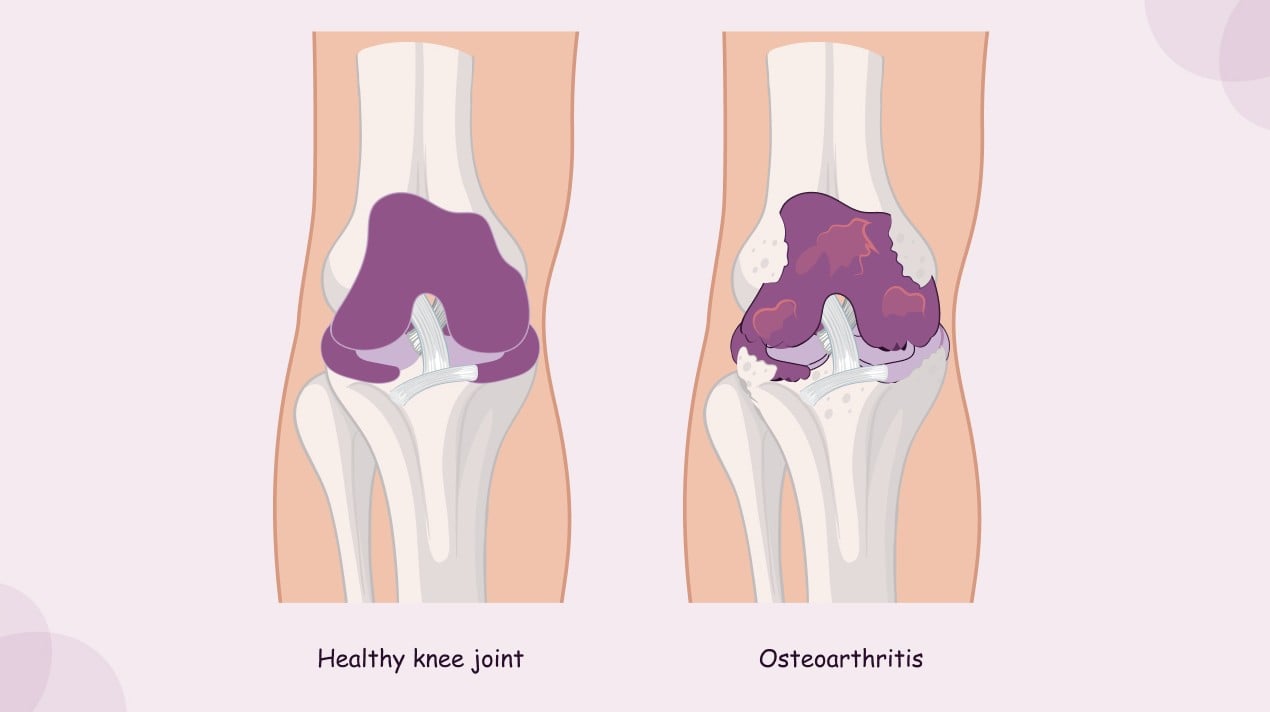
Osteoarthritis is a degenerative joint disease that primarily affects the cartilage — the smooth, rubbery tissue that cushions the ends of bones in the joint. Over time, the cartilage breaks down due to excessive strain from poor posture, weak muscles, or repetitive use, especially as we age. This leads to increased friction between the bones in the knee, causing pain, swelling, stiffness, and a reduced range of motion. As the cartilage wears down further, it can lead to the formation of bony growths (bone spurs), which can exacerbate pain and discomfort.
What Causes Osteoarthritis in the Knee?
Several factors contribute to the development of osteoarthritis in the knee:
- Aging: As you age, the cartilage in your knee naturally wears down. This makes the bones in the knee joint more susceptible to friction, leading to pain and stiffness.
- Poor Posture and Weak Muscles: Abnormal posture or muscle weakness can place excessive strain on the knee joint. Over time, this strain can wear down the cartilage and lead to osteoarthritis.
- Repetitive Stress: Activities that involve repeated knee bending, twisting, or high-impact movements (such as running, sports, or lifting) can place undue stress on the knee joint, contributing to cartilage breakdown.
- Obesity: Excess body weight puts additional strain on the knees, accelerating the wear and tear of the cartilage. This is a major risk factor for developing osteoarthritis in the knee.
- Previous Injuries: Injuries like fractures, ligament tears, or meniscus damage can increase the likelihood of developing osteoarthritis later in life, as they can disrupt the normal function of the joint.
What Health Conditions Can Osteoarthritis Lead to?
Osteoarthritis in the knee can also lead to or exacerbate other health conditions, including:
- Meniscus Tear: The meniscus is a cartilage structure in the knee that acts as a cushion between the femur and tibia. Osteoarthritis can weaken the meniscus, making it more prone to tears. A torn meniscus can further contribute to knee pain and instability.
- Rheumatoid Arthritis: Though primarily an autoimmune condition, rheumatoid arthritis can also affect the knee joint. When rheumatoid arthritis and osteoarthritis coexist, the combined effect can significantly worsen symptoms like pain, swelling, and stiffness.
- Gout and Pseudogout: Gout is a form of inflammatory arthritis caused by the buildup of uric acid crystals in the joints, while pseudogout is similar but caused by calcium pyrophosphate crystals. Both conditions can cause sudden and severe pain, often affecting the knee, and can be exacerbated by the presence of osteoarthritis.
- Septic Arthritis: Although rare, septic arthritis occurs when an infection enters the joint, causing inflammation, pain, and swelling. This condition can occur alongside osteoarthritis, particularly in individuals with weakened immune systems or those who have had knee surgeries.
What Are the Symptoms of Osteoarthritis in the Knee?
The symptoms of knee osteoarthritis can vary depending on the severity of the condition but typically include:
- Pain: Pain is the hallmark symptom of osteoarthritis in the knee. This pain often worsens with activity, such as walking, climbing stairs, or standing for prolonged periods. In advanced stages, pain may occur even at rest.
- Stiffness: People with knee osteoarthritis often experience stiffness, particularly after sitting or lying down for extended periods. This stiffness can make it difficult to fully bend or straighten the knee.
- Swelling: Swelling in the knee can occur as a result of inflammation or the formation of bone spurs. This can further limit the knee’s range of motion.
- Reduced Mobility: As the cartilage wears down, the knee joint becomes less flexible. This leads to difficulty with activities that involve bending or straightening the knee, such as walking or standing up from a seated position.
- Grating Sensation: In some cases, individuals with knee osteoarthritis may experience a grating or crunching sensation in the knee as the rough surfaces of the bones rub together.
How is Osteoarthritis in the Knee Diagnosed?
To diagnose osteoarthritis, a healthcare provider will typically begin with a physical exam to assess the range of motion, tenderness, and swelling in the knee. Imaging tests such as X-rays and MRI scans can provide detailed images of the knee joint and help confirm the presence of cartilage damage, bone spurs, or other structural changes indicative of osteoarthritis.
How is Osteoarthritis in the Knee Treated?
While osteoarthritis cannot be cured, several treatments can help manage symptoms and improve joint function:
- Physical Therapy: Strengthening the muscles surrounding the knee, especially the quadriceps and hamstrings, can help support the joint and reduce the strain on the cartilage. Stretching exercises can also improve flexibility and reduce stiffness.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help reduce pain and inflammation. In more severe cases, corticosteroid injections may be used to provide temporary relief.
- Weight Management: Losing weight can significantly reduce the strain on the knees, helping to alleviate pain and slow the progression of osteoarthritis.
- Bracing and Assistive Devices: Knee braces or sleeves can provide support and stability to the joint, while assistive devices like canes can help reduce the load on the knee during walking.
- Surgical Options: In cases of severe osteoarthritis, when conservative treatments are ineffective, surgical options may be considered. These include:
- Arthroscopy: A minimally invasive procedure that allows doctors to clean out damaged tissue or remove bone spurs.
- Partial Knee Replacement: If only one part of the knee is affected, a partial knee replacement may be performed to replace the damaged part of the joint.
- Total Knee Replacement: In severe cases, a total knee replacement may be necessary to replace the entire knee joint with a prosthesis.
How Can Osteoarthritis in the Knee Be Prevented?
While osteoarthritis is a degenerative condition associated with aging, several measures can help prevent or slow its progression:
- Exercise Regularly: Regular low-impact exercise, such as swimming, cycling, or walking, can strengthen the muscles around the knee and improve flexibility, helping to support the joint and reduce stress on the cartilage.
- Maintain a Healthy Weight: Excess body weight can put added strain on the knee joints, accelerating the wear and tear of cartilage. Maintaining a healthy weight can help reduce the risk of developing osteoarthritis.
- Use Proper Posture and Technique: When engaging in physical activities like running, lifting, or squatting, using proper form and technique can help prevent excessive strain on the knee joint.
- Avoid High-Impact Activities: Repeated high-impact activities, such as running on hard surfaces, can increase the risk of developing osteoarthritis. Opt for low-impact exercises whenever possible.
Conclusion: Managing Osteoarthritis in the Knee
Osteoarthritis in the knee can be a debilitating condition, but with the right treatment and lifestyle adjustments, it is possible to manage symptoms and improve quality of life. If you’re experiencing persistent knee pain or difficulty with mobility, it’s important to consult with a healthcare provider for a proper diagnosis and treatment plan. By addressing the issue early and taking proactive steps to protect your knee joints, you can help prevent further damage and maintain your knee health for years to come.
References
- Felson, D. T., & Lawrence, R. C. (2000). Osteoarthritis: Epidemiology and risk factors. Rheumatic Disease Clinics of North America, 26(3), 535-552. Available at: https://pubmed.ncbi.nlm.nih.gov/10986591/
2. Lo, G. H., & Lu, J. (2004). Osteoarthritis and its management. Journal of Orthopaedic Surgery and Research, 12(4), 12-16. Available at: https://pubmed.ncbi.nlm.nih.gov/17302874/
3. McAlindon, T. E., & Bannuru, R. R. (2017). Nonpharmacologic management of osteoarthritis. American Journal of Preventive Medicine, 53(3), S1-S7. Available at: https://pubmed.ncbi.nlm.nih.gov/28688772/