Knee pain can make everyday activities feel like a challenge, and if you’re experiencing persistent discomfort in the knee, patellar instability might be the culprit. The patella, or kneecap, plays a critical role in knee movement by gliding smoothly along a groove in the femur (thigh bone). However, when the patella moves out of its normal position, it can cause pain, discomfort, and difficulty with knee mobility. This blog will delve into what causes patellar instability, the associated health conditions, and how it can be treated effectively.
What is Patellar Instability?
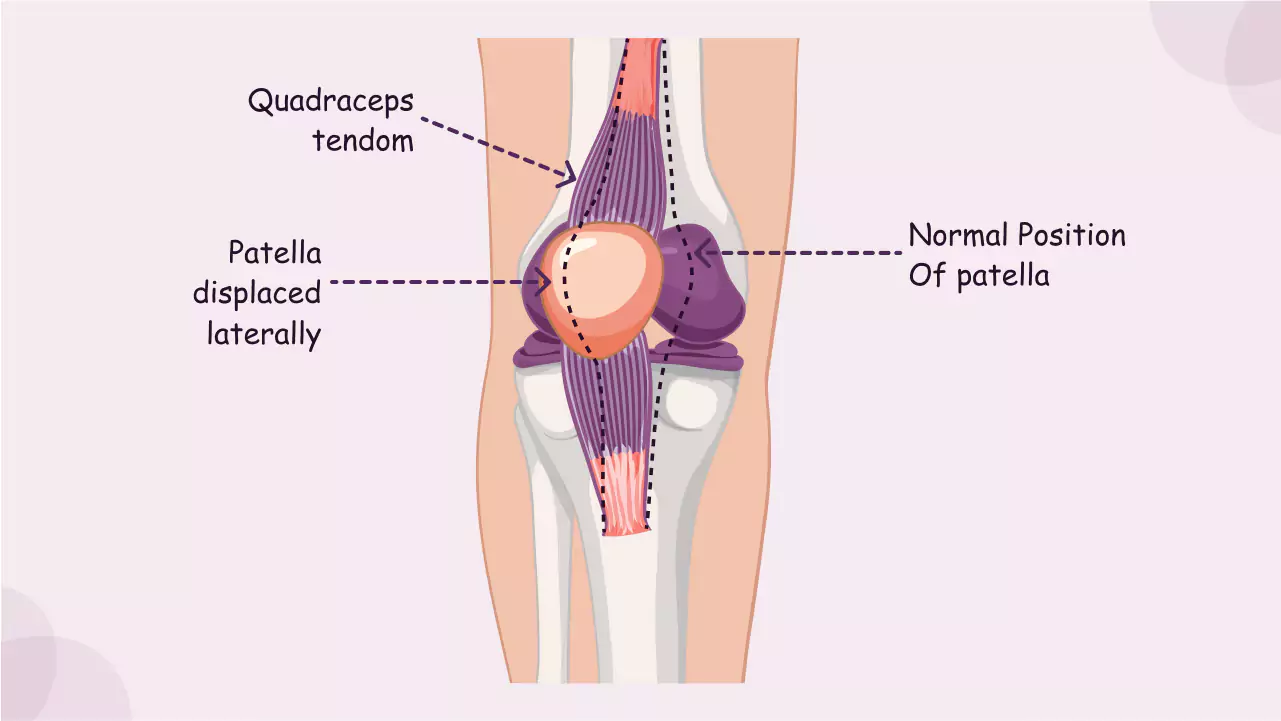
Patellar instability refers to the inability of the kneecap to stay within its natural position on the femur, leading to misalignment, pain, and difficulty moving the knee properly. The patella typically moves smoothly within a groove at the end of the femur called the trochlear groove. However, if the patella is displaced or moves incorrectly, it can cause significant discomfort and, in some cases, knee instability.
There are two primary forms of patellar instability:
- Patellar Dislocation: The patella completely shifts out of the groove, usually to the outside of the knee, causing severe pain and immobility.
- Patellar Subluxation: This occurs when the patella partially displaces but does not fully come out of place, leading to a sense of instability or “looseness” in the knee.
What Causes Patellar Instability?
Several factors can contribute to patellar instability. These include:
- Weak or Imbalanced Thigh Muscles: The quadriceps muscle group plays a crucial role in stabilizing the patella. If the quadriceps, particularly the inner part (vastus medialis), are weak or imbalanced, they may not properly guide the patella within its groove. This imbalance can lead to maltracking and instability.
- Repetitive Stress: Activities that involve frequent knee bending, twisting, or jumping (like running, cycling, or playing sports) can place repetitive stress on the patella. Over time, this stress can cause the patella to shift out of alignment, leading to instability.
- Trauma or Injury: A fall, direct blow to the knee, or other forms of trauma can cause the patella to dislocate or subluxate. Ligament injuries, especially damage to the medial patellofemoral ligament (MPFL), which helps keep the patella in place, can also make the knee more prone to instability.
- Structural Abnormalities: Some individuals may be born with a shallow trochlear groove or other anatomical differences that make it easier for the patella to move out of place. Abnormalities in the alignment of the lower leg bones, such as overpronation or a high-riding patella, can also increase the risk of instability.
- Previous Dislocations: Once the patella has dislocated, the tissues and ligaments around the knee can become stretched or weakened. This increases the likelihood of future dislocations or subluxations.
What Health Conditions Can Patellar Instability Lead To?
Patellar instability can manifest into several health conditions if not properly addressed, including:
- Patellar Maltracking: This occurs when the patella moves out of its normal alignment during knee motion. Maltracking can cause pain, discomfort, and increased wear on the knee joint, potentially leading to chondromalacia patella, where the cartilage under the kneecap breaks down.
- Chondromalacia Patella: This condition occurs when the cartilage behind the patella begins to wear away due to abnormal tracking. The friction between the patella and the femur can cause pain, swelling, and difficulty bending or straightening the knee. It often results from maltracking and can worsen over time if not treated.
- Patellar Dislocation: A complete displacement of the patella from the femoral groove can occur during activities like twisting or sudden changes in direction. This is often accompanied by intense pain, swelling, and an inability to move the knee properly. Recurrent dislocations can cause long-term knee instability and damage to the surrounding tissues.
- Patellar Subluxation or Dislocation: While a subluxation involves partial displacement of the patella, a dislocation refers to a complete shift out of place. Both conditions can result in repeated episodes of instability and pain, especially if they are not adequately treated.
What Are the Symptoms of Patellar Instability?
Patellar instability is marked by several noticeable symptoms, including:
- Pain in the Front of the Knee: Individuals with patellar instability often experience pain in the front of the knee, especially when performing activities that involve knee bending, such as climbing stairs or sitting for long periods.
- Knee “Giving Way” or Feeling Loose: Those with patellar instability often report a sensation of the knee giving way or feeling unstable. This is due to the patella’s improper tracking or partial displacement.
- Swelling: A dislocated or subluxated patella can cause swelling around the knee joint. Swelling can also be present in cases of repeated subluxation or maltracking.
- Difficulty with Knee Movement: The pain and instability may make it difficult to fully bend or straighten the knee, limiting mobility and function.
How is Patellar Instability Diagnosed?
A healthcare provider can diagnose patellar instability through a physical examination, where they may manipulate the knee to assess for instability or abnormal patellar movement. Imaging tests like X-rays and MRI scans are often used to assess any structural damage to the patella, cartilage, or surrounding tissues. These tests can also help rule out other potential causes of knee pain, such as fractures or arthritis.
How is Patellar Instability Treated?
Treatment for patellar instability typically begins with conservative methods, which may include:
- Physical Therapy: Strengthening the quadriceps, especially the vastus medialis muscle, is essential for improving patellar tracking and stability. Therapy may also focus on correcting muscle imbalances and improving flexibility in the hips and lower legs.
- Bracing: A knee brace or patellar stabilizer may be used to provide additional support and prevent the patella from shifting out of place during activity. Bracing can help reduce pain and prevent further instability.
- Activity Modification: Reducing high-impact activities or movements that exacerbate instability, such as jumping, squatting, or twisting, can help minimize pain and allow the knee to heal.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation. Corticosteroid injections may be used in more severe cases to provide temporary relief.
- Surgery: In cases where conservative treatments fail, surgical intervention may be necessary. Procedures may include lateral release (cutting tight tissue on the outside of the knee), MPFL reconstruction (repairing or reconstructing the ligament that stabilizes the patella), or realignment of the patella.
How Can Patellar Instability Be Prevented?
Preventing patellar instability involves strengthening and maintaining flexibility in the muscles surrounding the knee, especially the quadriceps. Here are some preventive measures:
- Strengthening Exercises: Focus on strengthening the quadriceps, hamstrings, and hip muscles to improve overall knee stability.
- Proper Form: Ensure that your posture and movement patterns during activities like running, squatting, or jumping are correct. Using proper form can help prevent unnecessary strain on the knee.
- Bracing During High-Risk Activities: If you engage in activities that place a lot of stress on the knees, such as sports or heavy lifting, consider using a knee brace to support the patella and prevent injury.
- Stretching: Stretching the hip flexors, calves, and hamstrings can help improve flexibility and reduce the risk of muscle imbalances that may contribute to patellar instability.
Conclusion: Taking Control of Patellar Instability
Patellar instability can significantly impact your quality of life, causing persistent knee pain and difficulty with movement. However, with early intervention and proper treatment, it is possible to manage the condition and regain full function of the knee. If you’re experiencing symptoms of knee instability or suspect patellar misalignment, it’s important to consult with a healthcare provider who can help diagnose the issue and recommend the appropriate course of treatment.
References
- Fithian, D. C., & Kelly, M. A. (2002). Patellar instability: Diagnosis and management. The Journal of Bone and Joint Surgery, 84(1), 75-80. Available at: https://pubmed.ncbi.nlm.nih.gov/11886897/
2. Ahn, J. H., & Kim, K. H. (2013). Patellar instability and its treatment. Sports Medicine and Arthroscopy Review, 21(3), 126-133. Available at: https://pubmed.ncbi.nlm.nih.gov/23965362/
3. Roush, G. K., & Cooley, D. M. (2011). Patellar instability and its clinical implications. Current Reviews in Musculoskeletal Medicine, 4(4), 1-7. Available at: https://pubmed.ncbi.nlm.nih.gov/23114734/