Have you been struggling with persistent neck pain that just won’t go away? You’re not alone. Many people experience chronic neck pain, and one of the leading causes of this discomfort is compressed nerves in the cervical spine. The spine plays a key role in linking your brain to your body, with 31 pairs of nerves branching from the spinal cord to control movement and sensation in your arms, legs, and trunk. When these nerves are compressed, it can result in a cascade of pain and other symptoms that affect your quality of life. In this blog, we will explore what compressed nerves in the neck are, how they can lead to chronic pain, and the health conditions associated with them.
What Causes Nerve Compression in the Neck?
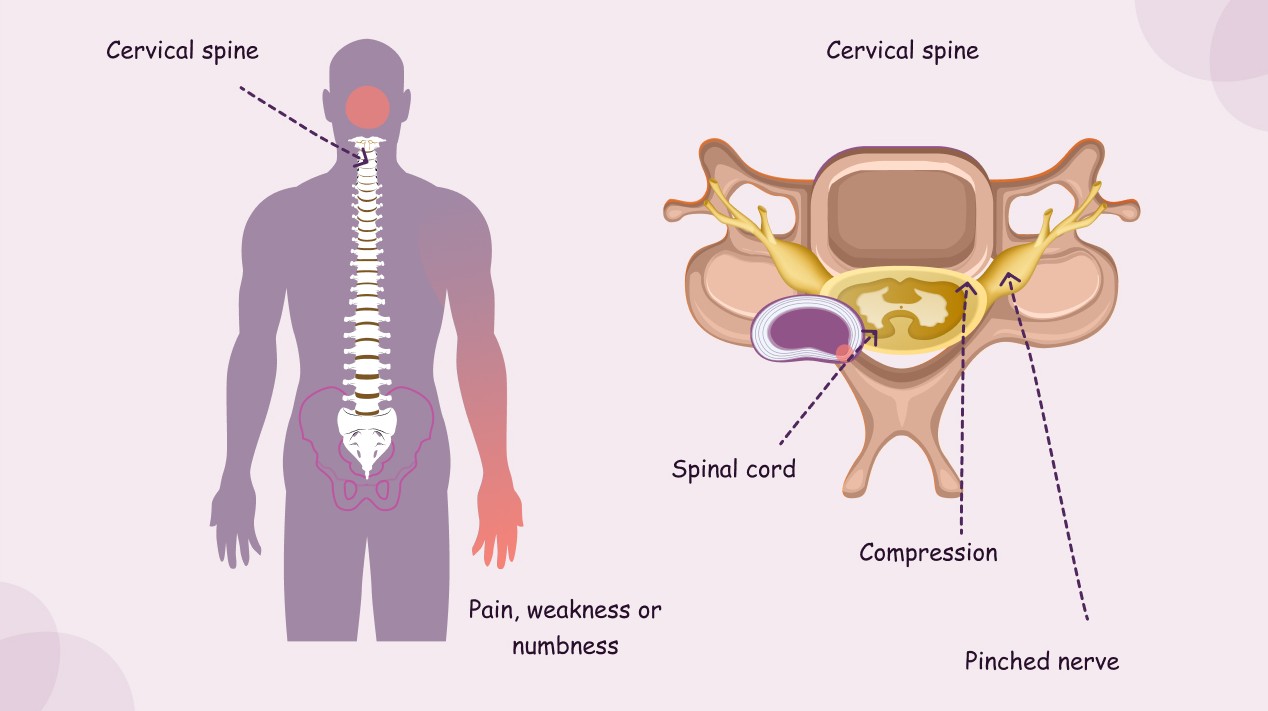
Your cervical spine, or the neck area of the spine, consists of seven vertebrae stacked on top of each other. These vertebrae protect the spinal cord, a major pathway linking your brain to the rest of your body. Between these vertebrae are soft discs that act as cushions, preventing the bones from rubbing against each other. When these discs wear down, become damaged, or slip out of place, they can press on the nerves that exit from the spinal cord, causing pain, numbness, or weakness in the neck and surrounding areas.
As we age, the bones, discs, and joints in the cervical spine undergo wear and tear, leading to conditions such as cervical disc degeneration. This natural aging process is often the root cause of nerve compression. But it can also happen due to an injury, bad posture, or repeated strain on the neck muscles. Conditions like a herniated disc or a narrowing of the spaces in the spine (spinal stenosis) can also lead to nerve compression.
How Does Nerve Compression Lead to Chronic Neck Pain?
When a nerve in the neck is compressed, it can cause inflammation and irritation, leading to pain. This pain may be localized to the neck, or it can radiate into the shoulders, arms, and hands. In some cases, the compression of nerves can cause muscle weakness, numbness, or a tingling sensation, often described as “pins and needles.”
Over time, this condition can worsen, and the pain may become chronic. You may find it difficult to turn your head, lift objects, or perform everyday tasks without discomfort. The pressure on the nerves can disrupt the normal function of the muscles and ligaments in the neck, causing stiffness and additional strain, which exacerbates the pain.
What Health Conditions Can Nerve Compression in the Neck Lead To?
Compressed nerves in the neck can contribute to several conditions that cause persistent pain and discomfort. Here are a few common health conditions associated with nerve compression:
- Ruptured (Herniated) Disc: A herniated disc occurs when the soft cushion-like material between the vertebrae slips out of place, putting pressure on nearby nerves. This can lead to sharp pain, numbness, or weakness in the neck and upper limbs (1).
- Cervical Stenosis: This condition refers to the narrowing of the spinal canal, which can compress the spinal cord and nerves. Cervical stenosis often occurs as a result of arthritis or degenerative changes in the spine, leading to chronic pain, stiffness, and tingling sensations in the arms and legs (2).
- Synovial Cyst: A synovial cyst is a fluid-filled sac that forms in the spine and can compress nearby nerves. Although rare, these cysts can cause neck pain, stiffness, and radiating pain that travels into the arms (3).
- Spinal Tumors: While less common, tumors in the cervical spine can put pressure on the spinal cord or nerves, leading to pain, numbness, and weakness. Tumors may be benign or malignant, and any persistent neck pain that doesn’t respond to traditional treatments should be evaluated by a healthcare professional (4).
How Do You Know If Compressed Nerves Are Causing Your Neck Pain?
If you have been dealing with neck pain that radiates into your arms, hands, or shoulders, or if you experience numbness or tingling sensations in these areas, nerve compression may be the cause. Other symptoms, such as muscle weakness, difficulty with balance, or a loss of coordination, should be taken seriously. If you are experiencing any of these symptoms, it’s crucial to consult a healthcare provider for a proper diagnosis.
A physical examination, along with imaging tests such as X-rays, MRIs, or CT scans, can help pinpoint the cause of nerve compression. Based on the diagnosis, your doctor will develop a treatment plan tailored to your condition.
What Are the Treatment Options for Nerve Compression?
Fortunately, most cases of nerve compression in the neck can be treated without surgery. The first step in treatment usually involves conservative measures such as:
- Physical Therapy: Specific exercises can help relieve pressure on the nerves by strengthening the muscles around the neck and improving posture (5).
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants can help reduce inflammation and relieve pain. In more severe cases, corticosteroid injections may be used to reduce swelling around the nerves (6).
- Heat and Ice Therapy: Applying heat or cold to the neck can help reduce pain and inflammation, providing temporary relief from nerve compression (7).
In cases where conservative treatments don’t provide relief, surgical options may be considered. Surgery might involve removing a portion of the disc or bone to relieve pressure on the affected nerve.
Conclusion: Addressing Nerve Compression in the Neck
Compressed nerves in the cervical spine are a common cause of chronic neck pain. Whether caused by wear and tear, a herniated disc, or other conditions, nerve compression can significantly affect your quality of life. Understanding the underlying cause of your neck pain and seeking timely treatment is crucial for relieving symptoms and preventing further complications.
If you are struggling with chronic neck pain that doesn’t improve with rest, don’t hesitate to consult a healthcare provider. Early intervention can help prevent the condition from worsening and allow you to live a more comfortable, pain-free life.
References
- Cohen, S. P., & Bhatia, A. (2020). Herniated disc and cervical radiculopathy: Diagnosis and management. Journal of Pain Research, 13, 137-145. Available at: https://pubmed.ncbi.nlm.nih.gov/31988932/
2. Bydon, M., & Gokaslan, Z. L. (2018). Cervical stenosis and its effect on the spinal cord. Journal of Neurosurgery: Spine, 28(6), 617-625. Available at: https://pubmed.ncbi.nlm.nih.gov/29695133/
3. Sharma, H., & Aggarwal, R. (2019). Synovial cysts and their role in cervical radiculopathy. Indian Journal of Orthopedics, 53(4), 474-478. Available at: https://pubmed.ncbi.nlm.nih.gov/30864243/
4. Barnett, R. (2017). Tumors of the cervical spine: A review. Journal of Spinal Disorders, 30(5), 413-420. Available at: https://pubmed.ncbi.nlm.nih.gov/27677518/
5. Dewar, A., & McAuley, J. (2017). Cervical radiculopathy and physical therapy: The role of conservative management. Journal of Rehabilitation Research and Development, 54(3), 569-574. Available at: https://pubmed.ncbi.nlm.nih.gov/28915452/
6. Jones, S., & John, R. (2018). Pharmacologic management of cervical radiculopathy. Journal of Pain Management, 11(1), 11-16. Available at: https://pubmed.ncbi.nlm.nih.gov/29414775/
7. Saini, S. S., & Pundir, S. (2020). Heat and ice therapy in managing cervical pain. Indian Journal of Pain Management, 34(2), 215-219. Available at: https://pubmed.ncbi.nlm.nih.gov/32053102/