Shoulder pain is something that many people experience at some point in their lives. One of the most frustrating and painful causes of chronic shoulder pain is frozen shoulder, a condition where the shoulder joint becomes stiff, painful, and difficult to move. Unlike other shoulder injuries, frozen shoulder gradually worsens over time and significantly limits mobility. In this blog post, we will explore what frozen shoulder is, its causes, symptoms, and how it can be treated.
What is Frozen Shoulder?
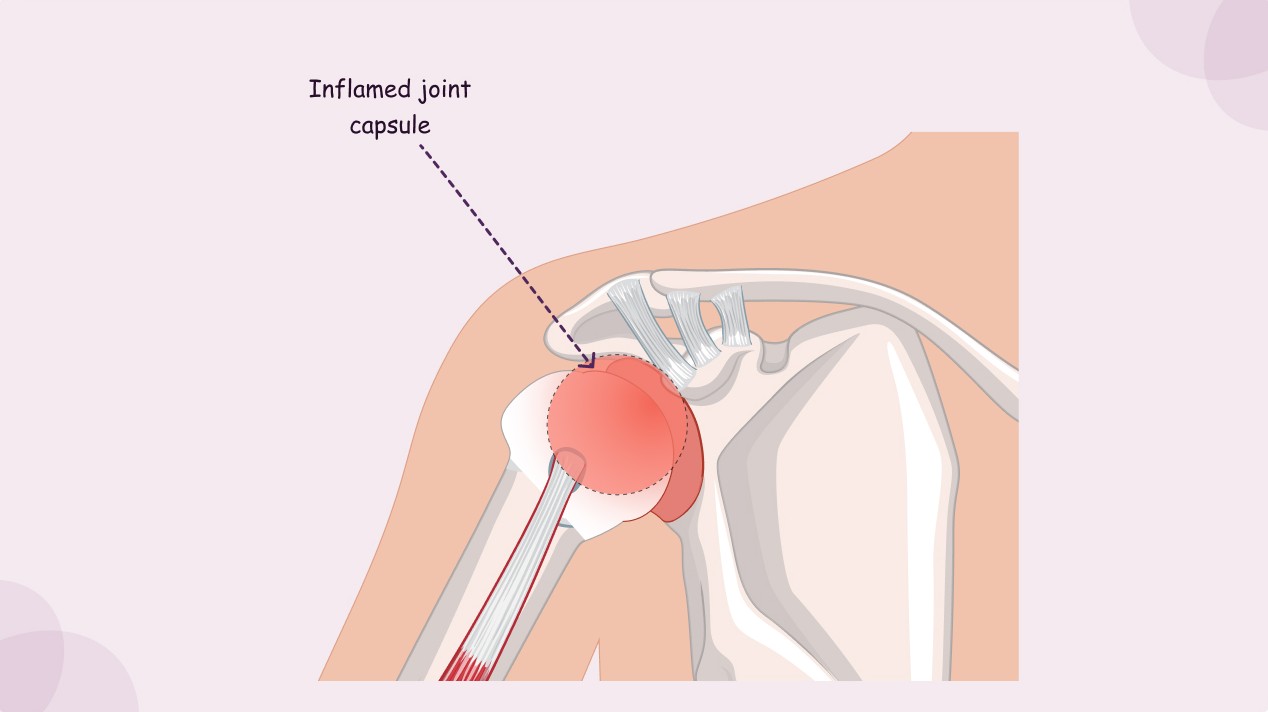
Frozen shoulder, also known as adhesive capsulitis, is a condition in which the shoulder joint becomes stiff, inflamed, and painful. The shoulder joint is a ball-and-socket joint that allows for a wide range of motion. In frozen shoulder, the capsule that surrounds the joint thickens and tightens, restricting movement. This results in pain, limited range of motion, and difficulty performing daily tasks that involve raising the arm or moving the shoulder.
Frozen shoulder usually develops in stages. It starts with mild pain, which gradually worsens over time. As the pain increases, the range of motion in the shoulder becomes more restricted. Over time, the shoulder may become “frozen,” meaning that even simple movements like reaching overhead or behind the back become extremely difficult and painful.
What Causes Frozen Shoulder?
Frozen shoulder can develop for a variety of reasons. The most common causes are:
- Prolonged Immobility: After an injury or surgery, if the shoulder remains immobile for a long period of time, it can trigger frozen shoulder. The lack of movement can cause the tissues around the shoulder joint to become tight and stiff, eventually leading to a loss of flexibility.
- Underlying Conditions: Certain health conditions can increase the risk of developing frozen shoulder. The most common condition linked to frozen shoulder is diabetes. People with diabetes are more likely to develop frozen shoulder, possibly due to changes in blood sugar levels that affect the connective tissues. Autoimmune disorders, such as thyroid disease or rheumatoid arthritis, can also trigger frozen shoulder due to inflammation in the body.
- Age and Gender: Frozen shoulder typically affects people between the ages of 40 and 60, and it is more common in women than men. As people age, the tissues around the shoulder joint naturally become less flexible, which may make them more prone to developing frozen shoulder.
- Trauma or Injury: A direct injury to the shoulder, such as a fall or accident, can also trigger frozen shoulder. After the injury, people may avoid using the shoulder to prevent pain, leading to the condition developing due to lack of movement.
What Are the Symptoms of Frozen Shoulder?
Frozen shoulder symptoms develop gradually and can be broken down into three stages:
- Freezing Stage (Painful Stage): This is the initial stage where pain begins. The pain is usually a dull or aching sensation, often felt on the outer shoulder and sometimes extending down the arm. It tends to worsen at night and can make it difficult to sleep on the affected side. The pain also becomes more intense when trying to move the arm.
- Frozen Stage (Stiffness Stage): After the freezing stage, the shoulder becomes stiffer, and the pain may begin to decrease slightly. However, the stiffness causes significant limitations in shoulder movement. People find it difficult to raise their arms or reach behind their back, and some everyday tasks like combing hair or putting on clothes become challenging.
- Thawing Stage (Recovery Stage): In this final stage, the stiffness begins to subside, and the range of motion in the shoulder slowly returns. The pain also decreases significantly, although some people may continue to experience discomfort for months. The recovery process can take anywhere from a few months to a couple of years, depending on the severity of the condition.
What Health Conditions Can Frozen Shoulder Lead To?
If left untreated, frozen shoulder can lead to a number of additional issues, including:
- Limited Mobility: As the shoulder becomes more stiff, it becomes difficult to perform basic movements, which can affect daily tasks. This can lead to further muscle weakness and dysfunction in the shoulder.
- Muscle Atrophy: Due to the lack of movement in the shoulder joint, the muscles surrounding the shoulder can weaken over time. This is known as muscle atrophy, and it can make it even harder to regain full function of the shoulder after the condition resolves.
- Chronic Pain: While the pain from frozen shoulder typically decreases during the thawing stage, some individuals may continue to experience lingering discomfort or stiffness. This can result in long-term discomfort and affect the quality of life.
- Impaired Functionality: Frozen shoulder can cause difficulties in performing activities that involve overhead movements, such as reaching for objects on a shelf, lifting, or playing sports. It can also hinder one’s ability to engage in physical exercise and can impact daily routines.
How is Frozen Shoulder Diagnosed?
Frozen shoulder is typically diagnosed through a physical examination by a healthcare professional. Your doctor will assess your range of motion, check for areas of tenderness, and evaluate how much pain is felt during shoulder movement. In some cases, the doctor may recommend imaging tests, such as X-rays or MRI scans, to rule out other possible causes of shoulder pain, like arthritis or rotator cuff injuries.
How is Frozen Shoulder Treated?
The treatment for frozen shoulder focuses on relieving pain, reducing inflammation, and restoring mobility to the shoulder joint. Some common treatments include:
- Physical Therapy: Physical therapy is the cornerstone of treatment for frozen shoulder. A physical therapist will guide you through exercises to help improve the range of motion and strengthen the muscles around the shoulder. Stretching exercises are often prescribed to help alleviate stiffness and encourage movement.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter medications like ibuprofen can help reduce pain and inflammation during the early stages of frozen shoulder.
- Corticosteroid Injections: In cases of severe pain, corticosteroid injections may be recommended to reduce inflammation and provide temporary relief.
- Heat and Cold Therapy: Applying heat or cold to the shoulder can help reduce pain and swelling. Cold packs can reduce inflammation, while heat can help relax tight muscles.
- Surgery: In rare cases, when other treatments fail, surgery may be considered. Manipulation under anesthesia is one option where the shoulder is moved while the patient is asleep to break up scar tissue. Arthroscopic surgery can also be performed to remove the thickened tissue from the shoulder joint.
Conclusion: Can You Prevent Frozen Shoulder?
While some risk factors, such as age or underlying health conditions, are beyond your control, there are steps you can take to reduce your risk of developing frozen shoulder. Staying active and maintaining good shoulder mobility through regular stretching and strengthening exercises can help keep your shoulder joint healthy. If you experience any pain or discomfort in your shoulder, it’s important to seek medical attention early to avoid prolonged immobility that can trigger frozen shoulder.
By addressing frozen shoulder early on, you can often prevent the condition from worsening and restore full function to your shoulder joint.
References
- Gall, M. M., & Yoon, S. (2019). Adhesive capsulitis (Frozen Shoulder): A review of diagnosis and treatment. Journal of Shoulder and Elbow Surgery, 28(3), 423-431. Available at: https://pubmed.ncbi.nlm.nih.gov/30553544/
2. Gaskill, T. R., & Dunn, W. R. (2018). Management of frozen shoulder. Sports Medicine and Arthroscopy Review, 26(4), 167-172. Available at: https://pubmed.ncbi.nlm.nih.gov/29905170/
3. Grewal, R., & Chaudhary, N. (2017). Frozen Shoulder: Pathophysiology and treatment. Indian Journal of Orthopaedics, 51(1), 18-23. Available at: https://pubmed.ncbi.nlm.nih.gov/28172488/
4. Favejee, M. M., & Huisman, M. (2020). Physical therapy for frozen shoulder: A systematic review. Journal of Rehabilitation Research, 58(2), 108-116. Available at: https://pubmed.ncbi.nlm.nih.gov/33019119/