Shoulder pain can feel like an obstacle in your everyday life, limiting your movement and impacting your ability to perform routine tasks. When the pain stems from osteoarthritis, it can become a persistent and frustrating condition. Osteoarthritis (OA) in the shoulder is a common cause of chronic pain, especially as you age. In this blog, we’ll explore how osteoarthritis develops in the shoulder, its causes, symptoms, and health conditions it may lead to, as well as effective treatment options.
What is Osteoarthritis in the Shoulder?
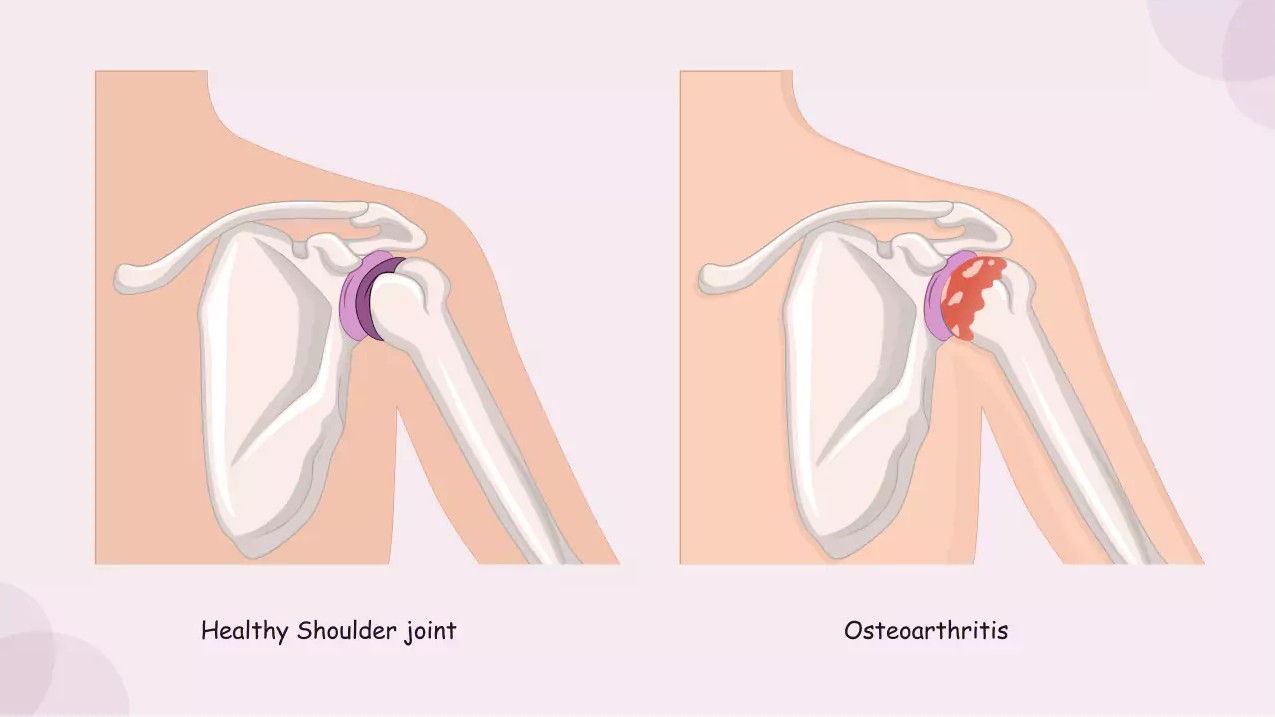
Osteoarthritis in the shoulder occurs when the cartilage in the shoulder joint begins to break down due to wear and tear. The shoulder joint is a ball-and-socket joint, where the head of the humerus (upper arm bone) fits into the shallow glenoid cavity of the scapula (shoulder blade). Healthy cartilage allows smooth movement by cushioning the bones and preventing friction. However, over time, excessive strain, poor posture, and muscle weakness can wear down the cartilage, causing pain, stiffness, and swelling.
This gradual breakdown can lead to painful bony growths, known as bone spurs, which make the condition worse. These spurs can further restrict movement and increase discomfort, making daily tasks like lifting objects or reaching overhead a challenge.
What Causes Osteoarthritis in the Shoulder?
Several factors can contribute to the development of osteoarthritis in the shoulder, with age being the most common. As you grow older, the cartilage in your joints naturally wears down. However, there are other factors that can accelerate this process:
- Excessive Strain: Poor posture, especially when sitting for long periods or slouching, places extra stress on the shoulder joints. Over time, this strain can contribute to cartilage breakdown. Repetitive overhead activities, such as lifting, throwing, or swimming, can also put additional stress on the shoulder joint and cause wear and tear.
- Weak Muscles: Weak muscles around the shoulder joint can fail to provide proper support, increasing the strain on the joint. Muscles help stabilize the joint, so when they are not functioning properly, the cartilage is more vulnerable to damage.
- Previous Injuries: A prior shoulder injury, such as a fracture or dislocation, can increase the risk of osteoarthritis. Injuries may disrupt the normal functioning of the joint and lead to uneven wear on the cartilage.
- Genetics: Some people may be genetically predisposed to developing osteoarthritis due to structural abnormalities in the joint or an inherited tendency for cartilage breakdown.
What Are the Symptoms of Osteoarthritis in the Shoulder?
Osteoarthritis in the shoulder manifests with several symptoms, which may develop gradually over time. These include:
- Pain: The most prominent symptom of osteoarthritis in the shoulder is pain. You may experience deep, aching pain in the shoulder joint, especially during movement. The pain tends to worsen after repetitive use or long periods of inactivity.
- Stiffness: As cartilage wears away, the shoulder joint becomes stiffer, making it difficult to fully rotate the arm or raise it overhead. This stiffness may also be more noticeable in the morning or after long periods of rest.
- Swelling and Inflammation: The breakdown of cartilage can cause inflammation in the joint, leading to swelling and warmth around the shoulder.
- Limited Range of Motion: Over time, the damage to the cartilage can reduce the shoulder’s range of motion. Tasks such as reaching behind your back or lifting objects overhead may become increasingly difficult.
- Crepitus: In some cases, people with shoulder osteoarthritis may experience a grinding or crackling sound (crepitus) when moving the shoulder joint. This sound occurs when the bones rub against each other due to the loss of cartilage.
What Health Conditions Can Osteoarthritis in the Shoulder Lead To?
If osteoarthritis is left untreated, it can lead to several complications and other health conditions, including:
- Glenohumeral Osteoarthritis: This is the most common form of osteoarthritis in the shoulder, affecting the ball-and-socket joint where the humerus (upper arm bone) fits into the glenoid (the socket of the shoulder blade). Over time, the cartilage in this joint breaks down, causing pain, stiffness, and limited motion.
- Acromioclavicular (AC) Joint Osteoarthritis: The acromioclavicular joint is where the collarbone (clavicle) meets the acromion (the top of the shoulder blade). AC joint osteoarthritis occurs when the cartilage in this area wears down, leading to pain at the top of the shoulder. This can also cause difficulty with lifting or reaching overhead.
- Bone Spurs: As the cartilage wears down, the body may respond by forming bone spurs (osteophytes), which are bony growths that develop along the edges of the joint. These spurs can further irritate the surrounding tissues and worsen pain and stiffness.
- Reduced Mobility: If the condition progresses without treatment, it can lead to permanent changes in the shoulder joint, reducing its ability to move and function properly. This can significantly affect quality of life and mobility.
How is Osteoarthritis in the Shoulder Diagnosed?
To diagnose osteoarthritis in the shoulder, a healthcare provider will typically perform a physical examination, where they assess the range of motion and check for signs of pain or tenderness. They may also use imaging tests, such as:
- X-rays: X-rays are often the first step in diagnosing osteoarthritis. They can show changes in the joint, including the narrowing of the joint space, bone spurs, and changes in the structure of the bones.
- MRI: An MRI (magnetic resonance imaging) provides a more detailed image of the soft tissues in the shoulder, including cartilage, muscles, and tendons. An MRI can help determine the extent of cartilage damage and the presence of any additional injuries.
How is Osteoarthritis in the Shoulder Treated?
Treatment for shoulder osteoarthritis typically involves a combination of non-surgical and, in more severe cases, surgical approaches. Some common treatment options include:
- Physical Therapy: Strengthening the muscles around the shoulder joint can provide better support, reducing stress on the cartilage. A physical therapist can guide you through specific exercises to improve the stability and range of motion of the shoulder.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter pain relievers, such as ibuprofen, can help reduce inflammation and pain associated with osteoarthritis.
- Corticosteroid Injections: For individuals with severe pain or inflammation, corticosteroid injections can provide temporary relief by reducing inflammation in the joint.
- Surgery: In advanced cases where conservative treatments are not effective, surgery may be necessary. Arthroscopy is a minimally invasive surgery that may be used to remove damaged cartilage or repair tissues. In more severe cases, a shoulder replacement (also called shoulder arthroplasty) may be recommended, where the damaged joint is replaced with a prosthetic.
Can Osteoarthritis in the Shoulder Be Prevented?
While osteoarthritis in the shoulder cannot always be completely prevented, there are several steps you can take to reduce the risk of developing the condition:
- Maintain a Healthy Weight: Excess weight puts added strain on your joints, increasing the risk of osteoarthritis. Keeping a healthy weight can help reduce this stress on the shoulder joint.
- Strengthen the Shoulder Muscles: Regular exercise to strengthen the muscles around the shoulder joint can help provide stability and prevent excessive wear on the cartilage.
- Improve Posture: Practicing good posture, especially while sitting or lifting, can help reduce the strain on your shoulder joints and prevent unnecessary wear and tear.
- Avoid Overuse: Repetitive movements, especially overhead activities, can increase the risk of shoulder osteoarthritis. Taking breaks and avoiding overuse can help preserve the joint.
Conclusion: Managing Osteoarthritis in the Shoulder
Osteoarthritis in the shoulder is a common cause of chronic pain, especially as we age. While it cannot be entirely prevented, there are several strategies to manage and reduce the symptoms of osteoarthritis. With early diagnosis and proper treatment, you can maintain shoulder function and reduce pain, allowing you to continue your daily activities with ease. If you suspect that you have shoulder osteoarthritis, it’s important to consult with a healthcare provider to determine the best treatment options for your specific condition.
References
- Murphy, L., & Helmick, C. G. (2012). The impact of osteoarthritis in the United States: A population-health perspective. The American Journal of Public Health, 102(5), 858-865. Available at: https://pubmed.ncbi.nlm.nih.gov/22390511/
2. McCarty, W. A., & Mishra, P. (2019). Osteoarthritis of the shoulder: Diagnosis and management. Orthopedic Clinics of North America, 50(4), 413-419. Available at: https://pubmed.ncbi.nlm.nih.gov/31410698/
3. Gaujoux, S., & Boutron, I. (2014). Surgical management of osteoarthritis of the shoulder: Outcomes and complications. The Journal of Shoulder and Elbow Surgery, 23(3), e43-e50. Available at: https://pubmed.ncbi.nlm.nih.gov/24211948/
4. Yamaguchi, K., & Dines, D. M. (2016). Shoulder osteoarthritis: Pathophysiology, diagnosis, and treatment. The Journal of Bone and Joint Surgery, 98(12), 970-978. Available at: https://pubmed.ncbi.nlm.nih.gov/27230719/