If your whole body has been feeling like it ran a marathon you don’t remember signing up for then welcome to the club. Everyone gets tired after a long day, or achy after sitting like a shrimp at their desk for hours. But when the tiredness becomes your personality and every joint suddenly wants its own mini protest, it’s time to stop blaming “age” (you’re 22, calm down) and look a little deeper.
This guide breaks down why body pain and constant tiredness happen, how doctors figure out the cause, and what you can realistically do at home without turning your life upside down. It also covers when it’s time to actually see a doctor and stop self-diagnosing based on memes and five frequently asked questions with clear answers backed by trusted sources.
What Do We Mean by “Body Pain” and “Tiredness,” Really?
Body pain = that dull, irritating, sometimes dramatic ache in your muscles or joints, anything from “my back has opinions today” to “why does my leg feel like a rusty hinge?”
Tiredness (fatigue) = the kind of exhaustion that doesn’t go away with one good night’s sleep. Or two. Or caffeine. It’s that feeling of dragging yourself through tasks that used to be easy, and wondering why your brain feels like it’s on low battery mode.
If these stick around for weeks instead of days, or start messing with your daily life, they’re worth paying attention to.
What Are the Most Common Causes of Body Pain and Tiredness?

Even though the list of causes looks long (and slightly scary), most cases fall into a few straightforward categories. Let’s break them down without the medical drama.
Lifestyle Habits: Are You Accidentally Stressing Out Your Body?
- Sometimes the cause isn’t deep rather it’s just life being life.
- Not sleeping well
- Sitting like a croissant all day
- Long hours at a desk without breaks
- Overtraining at the gym (yes, that counts too)
- Too much caffeine, not enough water
- Those long doom-scrolling nights at 2 AM
These habits alone can make your body ache and your energy drop to zero. And no, your mattress isn’t always the villain though a cervical pillow that actually supports your neck can be a lifesaver when posture is part of the problem.
(betterhood Cervical Pillow link): https://shop.betterhood.in/collections/cervical-pillows?
Medical Causes: When Your Body Is Saying “Please Investigate This”
Some conditions bring BOTH pain and tiredness the iconic duo nobody asked for.
- Fibromyalgia (1)
A chronic condition where your body mismanages pain signals. Everything hurts but nothing looks “wrong” on scans. Very common, very misunderstood.
- ME/CFS – Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (2)
Fatigue so deep that rest doesn’t fix it. Often triggered after infections. Comes with brain fog, body pain, and energy crashes.
- Arthritis & Autoimmune Conditions
Inflammation in joints = pain + full-body tiredness.
- Infections
Covid, mono, viral fevers can leave behind a “post-viral hangover” that lasts weeks.
Nutritional Deficiencies: Yes, Your Vitamins Matter
Low levels of:
- Iron → anemia → tired + weak
- Vitamin B12 → nerve-related fatigue
- Magnesium → cramps + weakness
- Vitamin D → muscle/bone pain and exhaustion (3)(4)
These deficiencies are surprisingly common especially Vitamin D, according to NCBI and Cleveland Clinic.
Mental Health & Sleep Disorders: The Invisible Contributors
Stress, anxiety, depression, they don’t just “affect mood.” They show up as:
- Body tension
- Poor sleep
- Fatigue
- Muscle pain
- Sleep apnea is another big one where you think you slept, but your body was basically fighting for air all night (5).
Environmental & Ergonomic Factors: Blame the Chair
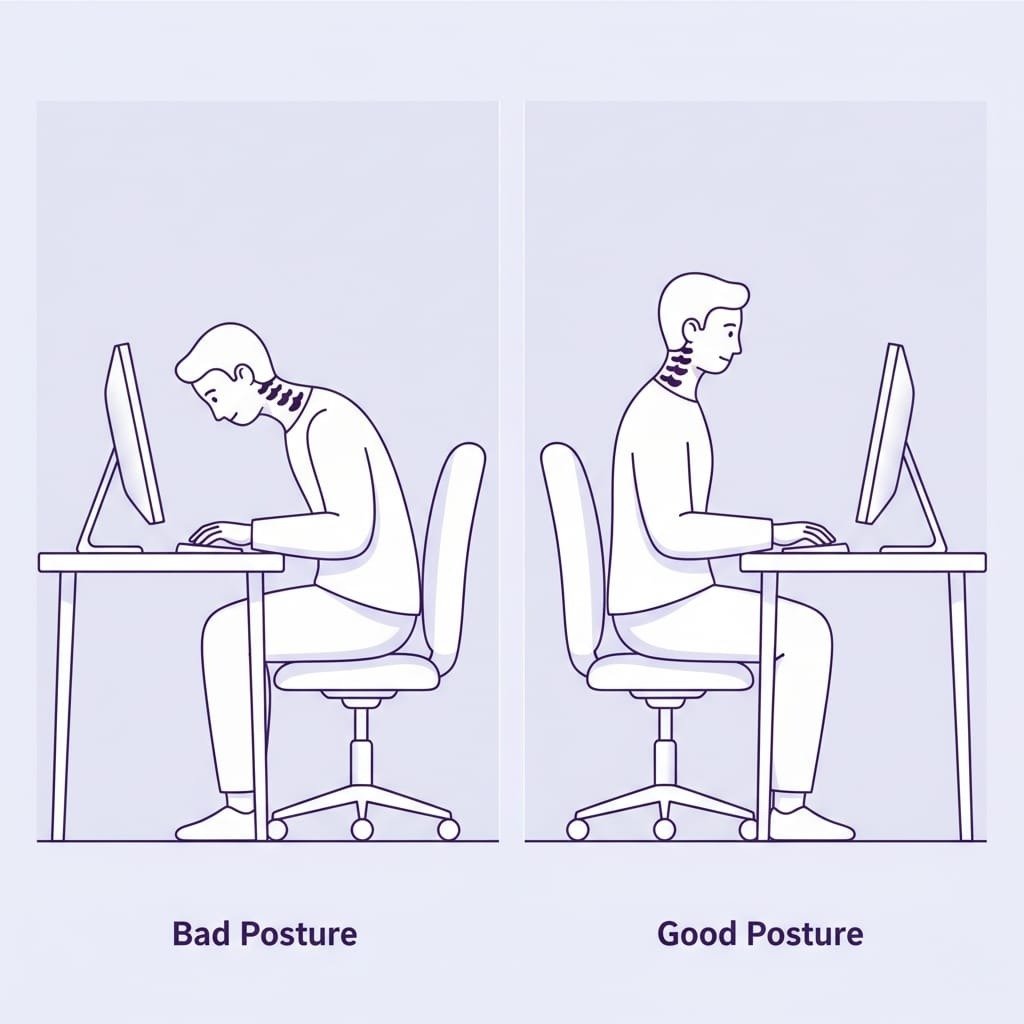
Bad workstation setups, terrible chairs, unsupportive mattresses, extreme AC temperatures, all of them can strain muscles over time. If your 9–5 involves sitting badly, start here.
Betterhood’s Lumbar Support Cushion is a solid upgrade if you want to stop fighting with your chair every day.
Link: https://shop.betterhood.in/products/betterhood-back-support-cushion-for-chair
What Symptoms Are Red Flags?
Most aches are harmless. BUT some symptoms need attention:
- Fatigue that refuses to improve for weeks
- Widespread muscle pain
- Swollen joints
- Brain fog that feels like your brain is buffering
- Snoring, gasping, or waking up exhausted
- Sudden weight changes
- Weakness that affects balance or walking
If you’re hitting these markers, don’t brush it off.
How Do Clinicians Figure Out What’s Going On?
A proper evaluation usually includes:
- Medical History
When did symptoms start, how dramatic are they, did they follow an infection, an injury, or a life meltdown?
- System Review
Sleep, mood, appetite, stress, medications, the whole picture.
- Physical Exam
Checking posture, strength, flexibility, neurological signs.
- Basic Blood Tests
CBC, thyroid panel, CRP/ESR, Vitamin D, B12, iron studies.
- Targeted Tests
MRI/X-ray if something structural is suspected, sleep studies for apnea, auto immune panels when needed.
- Referrals
Rheumatology, neurology, sleep medicine, depending on the clues.
For conditions like fibromyalgia and ME/CFS, diagnosis is clinical. There’s no single magic test.
What Home Strategies Actually Help Without Making You Miserable?
Here’s the good news, many people improve A LOT with small, consistent habits
How Can You Improve Sleep Quality?
- Keep a fixed sleep routine
- Limit screens before bed
- Create a calmer wind-down process
- If snoring or choking in sleep → discuss a sleep study
(Apnea is sneaky. Exhaustion is its love language.)
What Nutrition and Hydration Changes Make a Difference?
- Eat balanced meals (protein, vegetables, whole grains)
- Monitor iron and vitamin levels if symptoms persist
- Drink more water your body gets cranky when dehydrated
Can Gentle Movement Really Reduce Pain?
Absolutely yes.
Even if your body feels like it’s made of noodles.
- Light walking
- Gentle yoga
- Stretching
- Movement breaks during long sitting periods
And if sore muscles are part of the problem, Betterhood’s Pain Relief Roll-On is a genuinely soothing option for quick relief:
Link: https://shop.betterhood.in/products/recovery-roll-on-with-menthol-magnesium-boswellia
For chronic conditions, a physiotherapist-led plan works better than forcing yourself through pain.
Does Stress Make Pain Worse?
Stress can turn tiny aches into dramatic sagas. Try:
- deep breathing
- Mindfulness
- muscle relaxation
- therapy (CBT works really well for chronic fatigue/pain)
Betterhood’s Gratitude + Mental Wellbeing article is a great read if your stress and fatigue often hold hands:
https://betterhood.in/learn/why-gratitude-boosts-mental-health-and-well-being/
Do Heat and Cold Help?
- Heat → muscle tension
- Ice → swelling or acute injury
- Epsom salt baths = vibes + relief
- Fix your chair & desk = saves your back long-term
When Do You Need Medical Treatment or Therapies?
If home strategies help then great.
If not, here’s what doctors usually consider:
- Medications & Supplements
- Pain relievers for flare-ups
- Iron/B12/Vitamin D if levels are low (6)
- Condition-specific treatments for arthritis, thyroid issues, etc.
Physical & Occupational Therapy
- Physios guide safe movement; OTs teach energy-saving habits.
Specialist Clinics
- Multidisciplinary care is helpful for fibromyalgia or ME/CFS.
Alternative Therapies
- Massage, acupuncture, mindfulness are supportive but not replacements for medical care.
What Does a Practical 2-Week Relief Plan Look Like?
A simple starter schedule:
Week 1
- Sleep 30 minutes earlier
- No screens 1 hour before bed
- 15–20 minutes of gentle movement
- Hydrate better
- Add leafy greens or fatty fish
- 5 minutes of deep breathing twice a day
Week 2
- Increase activity slightly
- Morning mobility routine
- Keep a simple symptom log
If fatigue is unchanged → book a primary care visit
When Should You See a Doctor Urgently?
Skip Google. Go straight to a doctor if you have:
- sudden weakness, numbness, or speech difficulty
- chest pain or shortness of breath
- unexplained fever with worsening pain
- loss of bladder/bowel control
For less urgent but persistent symptoms (over 2–4 weeks), schedule a routine evaluation
Conclusion
Body pain and tiredness happen to everyone but they’re not meant to be permanent roommates. Small, steady lifestyle shifts often help more than dramatic overhauls. But if symptoms stick around, it’s worth checking for medical causes like anemia, thyroid issues, autoimmune conditions, fibromyalgia, or ME/CFS.
You don’t have to figure it all out alone. A good clinician + a realistic plan = actual progress.
Explore More Health & Wellness Solutions
If you want to understand your body better (and give it fewer reasons to protest), these Betterhood articles are great next reads:
Why Foam Rolling Helps Sore Muscles + How to Do It Right
https://betterhood.in/learn/foam-roller-exercises/
Posture Tips That Actually Reduce Neck & Back Strain
5 Subtle Signs Your Knees Are Asking for Help
https://betterhood.in/learn/signs-your-knees-need-help/
Frequently Asked Questions:
1. What most commonly causes constant body pain and tiredness?
Constant pain and persistent tiredness commonly arise from a combination of lifestyle factors (poor sleep, inactivity), underlying medical conditions (fibromyalgia, ME/CFS, arthritis, thyroid disease), and nutritional deficiencies (iron, vitamin D). Psychological stress and poor ergonomics also play major roles. If symptoms are new and lingering, medical evaluation helps identify the cause.
2. Can vitamin D deficiency cause muscle pain and fatigue?
Yes, low vitamin D is associated with muscle weakness, bone pain, and sometimes generalized fatigue. Testing and targeted supplementation guided by a clinician can improve symptoms for many people with documented deficie
3. How should I decide between home care and seeing a doctor?
Start with consistent self-care: sleep hygiene, hydration, balanced diet, gentle daily activity, and stress reduction. If symptoms fail to improve after two weeks, worsen, or are accompanied by red-flag signs (fever, weight loss, neurological changes), see a clinician for tests and targeted treatment.
4. Will exercise make my pain or fatigue worse?
Moderate, graded exercise usually helps. However, for conditions like ME/CFS that include post-exertional malaise, exercise must be very carefully paced and supervised; overdoing it can cause setbacks. For most people without those diagnoses, a progressive increase in gentle activity reduces pain and increases stamina.
5. Are there specific tests that diagnose chronic fatigue or fibromyalgia?
There is no single definitive lab test for fibromyalgia or ME/CFS; diagnosis is clinical and often involves ruling out other causes (blood tests, imaging). For fibromyalgia, clinicians use symptom history, widespread pain criteria, and evaluation of tender points; for ME/CFS, diagnostic criteria focus on persistent, debilitating fatigue for at least six months and post-exertional symptom worsening.
References
1.MayoClinic–Fibromyalgia https://www.mayoclinic.org/diseases-conditions/fibromyalgia/symptoms-causes/syc-20354780
2. CDC – ME/CFS Basics https://www.cdc.gov/me-cfs/about/index.html
3. NCBI – Vitamin D Deficiency https://www.ncbi.nlm.nih.gov/books/NBK532266
4. Cleveland Clinic – Vitamin D Deficiency https://my.clevelandclinic.org/health/diseases/15050-vitamin-d-vitamin-d-deficiency
5. NHS – Tiredness & Fatigue https://www.nhs.uk/symptoms/tiredness-and-fatigue
6. StatPearls – Vitamin D Deficiency (2025) https://www.ncbi.nlm.nih.gov/books/NBK532266























