Tailbone pain or coccydynia is a common yet often overlooked condition that affects the small bone at the base of the spine i.e the coccyx. Despite its size, the tailbone supports stability and balance while sitting, standing or bending. When pain occurs even simple move can become uncomfortable while minor pain may resolve on its own, persistent discomfort often signals underlying problems such as injuries, poor posture, childbirth, obesity or in rare cases as infection and tumors [1]. You should understand the reasons behind tailbone is essential for effective treatment and prevention. This article explores the anatomy of the coccyx and common causes of coccydynia and key factors to consider for better care and management.
Anatomy of the Tailbone (Coccyx)
The coccyx or tailbone, is a small triangular bone at the base of the spine, made up of three to five fused vertebrae. Though considered vestigial, it plays key roles in posture and movement.
Structure and Location
Located just below the sacrum, the coccyx is connected by the sacro-coccygeal joint and is vulnerable to pressure or injury, especially when sitting or falling.
Role in Sitting Posture
The coccyx supports body weight while sitting, working with the sitting bones to distribute pressure. Injury or inflammation can make sitting painful and lead to compensatory postures that affect the back and hips.
Connections to Muscles, Ligaments, and Nerves
It serves as an attachment point for the gluteus maximus, pelvic floor muscles, and ligaments that support bowel and bladder function. Surrounded by sensitive nerve endings, even minor issues can cause significant pain.
Common Reasons for Tailbone Pain
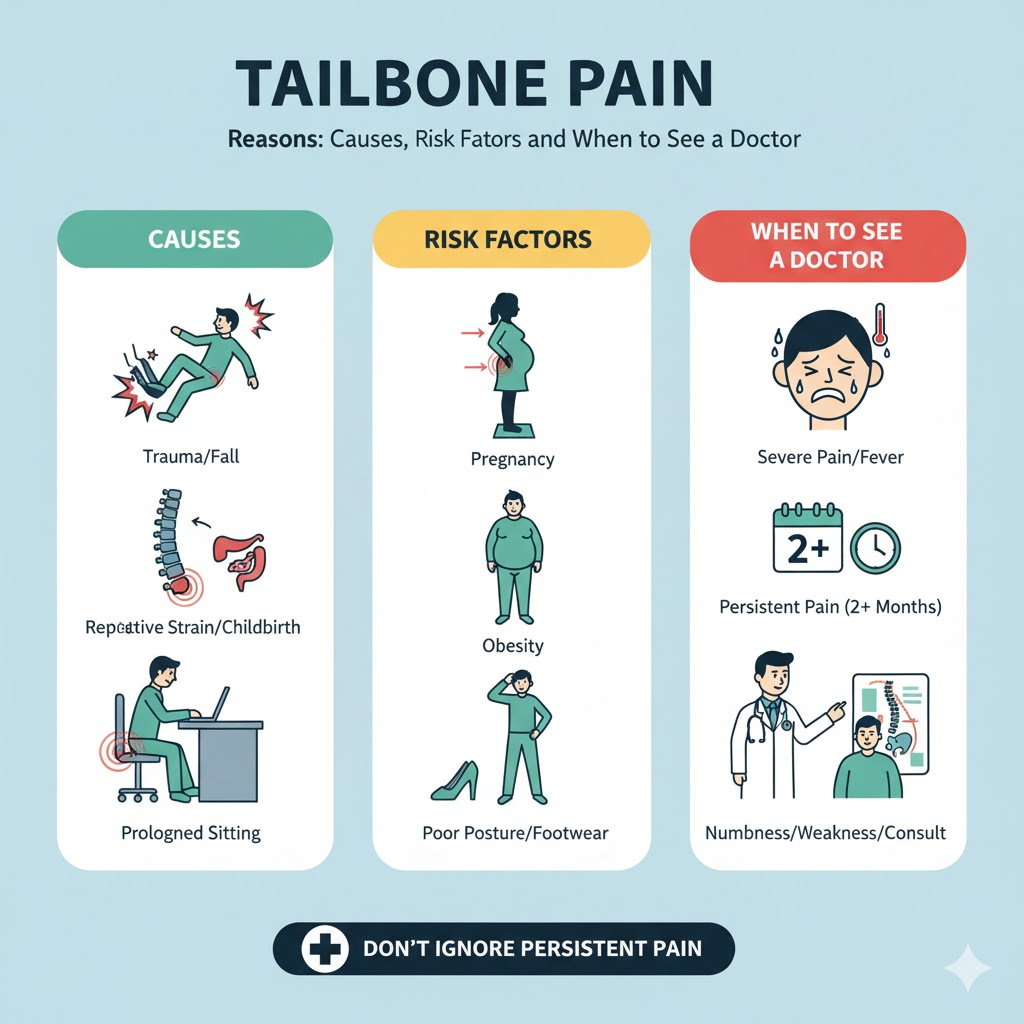
Tailbone pain (coccydynia) can stem from trauma, lifestyle habits, medical conditions, or physiological changes such as pregnancy.
Traumatic Causes
- Falls or Direct Injury: Landing on the buttocks may bruise, dislocate, or fracture the coccyx.
- Sports Injuries: Activities like cycling, skating, or contact sports increase risk
- Fractures/Dislocation: Severe trauma can cause sharp pain and long-term discomfort.
Non-Traumatic Causes
- Prolonged Sitting: Hard surfaces or long hours at desks increase pressure on the coccyx.
- Poor Posture: Slouching or leaning strains the coccyx with time.
- Repetitive Strain: Frequent bending or lifting may lead to irritation.
Pregnancy and Childbirth
- Hormonal Changes: Relaxin loosens ligaments, making the coccyx vulnerable.
- Delivery Pressure: Vaginal birth may bruise or dislocate the coccyx.
- Postpartum Pain: Misalignment or ligament laxity can cause lingering discomfort.
Obesity and Weight Issues
- Excess Weight: Adds pressure on the coccyx.
- Low Body Weight: Reduces natural cushioning, causing pain.
Degeneretive & Age-Related Factors
- Arthritis: Joint wear leads to stiffness and inflammation.
- Aging: Fragile bones increase fracture risk, and sitting worsens degeneration.
Infections & Tumors
- Infections (e.g., pilonidal cysts): Cause swelling, redness, and severe pain.
- Tumors: Rare, but persistent unexplained pain may signal cancer in the region [2].
Risk Factors for Tailbone Pain
Not everyone experiences tailbone pain, but certain risk factors make individuals more susceptible. Recognizing these risk factors can help in prevention and early intervention.
Gender Differences: Why Women are More Prone
Studies consistently show that women are more likely to experience coccydynia compared to men. Reasons include:
- Pregnancy and Childbirth – As explained earlier, hormonal changes and vaginal deliveries increase risk.
- Higher Pelvic Mobility – Women generally have greater pelvic flexibility, which may sometimes destabilize the sacrococcygeal joint.
Age-Related Vulnerability
While coccyx pain can occur at any age, certain patterns emerge:
- Children and Teens – More likely to injure their coccyx due to active play and sports.
- Adults (30–50 years) – Commonly affected due to prolonged sitting (work-related) or lifestyle habits.
- Older Adults – More prone to fractures due to weaker bones, osteoporosis, and degenerative joint conditions.
Lifestyle and Occupational Risk Factors
Modern lifestyles contribute significantly to coccyx discomfort:
- Sedentary Work – Office workers, drivers, and students who sit for long hours without breaks are highly at risk [3].
- Athletes in High-Risk Sports – Rowing, cycling, skating, and horseback riding put repetitive stress on the coccyx.
- Poor Ergonomics – Working on poorly designed chairs or desks contributes to poor posture and coccyx strain.
Medical and Physiological Risk Factors
- Obesity – Excess weight increases pressure on the coccyx during sitting.
- Being Underweight – Lack of natural fatty padding around the tailbone can make sitting painful.
- Osteoporosis – Weak bones fracture more easily, including the coccyx.
- Chronic Joint or Spinal Conditions – People with arthritis, lower back pain, or degenerative spinal issues are more prone to coccyx pain.
Symptoms and Associated Conditions
Tailbone pain can manifest in different ways depending on the underlying cause. Recognizing the full range of symptoms is essential for proper diagnosis.
Primary Symptoms of Tailbone Pain
- Localized Pain at the Base of the Spine – The most common symptom is aching, soreness, or sharp pain in the coccyx region.
- Worse When Sitting – Pain increases when sitting on hard surfaces or leaning backward.
- Pain During Position Changes – Moving from sitting to standing, bending, or climbing stairs may trigger pain.
- Tenderness on Touch – Applying pressure to the coccyx can cause noticeable discomfort.
Associated Symptoms
- Radiating Pain – In some cases, pain may extend to the lower back, hips, or buttocks.
- Difficulty Sleeping – Lying on the back may worsen discomfort, affecting rest quality.
- Stiffness and Limited Mobility – Chronic pain may lead to reduced pelvic flexibility.
- Pain During Bowel Movements – Due to coccyx involvement with pelvic floor muscles.
- Pain During Sexual Intercourse – Particularly in women, coccyx issues can cause discomfort during intimacy.
When to See a Doctor
While mild coccyx pain often improves with home care, there are situations where medical attention is necessary. Knowing when to seek professional help can prevent complications.
Red Flags for Immediate Medical Attention
- Severe Trauma – If pain follows a major fall, accident, or sports injury.
- Inability to Sit or Walk – Suggesting fracture or severe dislocation.
- Signs of Infection – Fever, swelling, pus, or redness near the tailbone area.
- Unexplained Weight Loss or Night Pain – Possible sign of tumors.
- Neurological Symptoms – Numbness, tingling, or weakness in legs may indicate nerve involvement.
Persistent Pain That Warrants Medical Review
- Pain lasting more than two weeks without improvement.
- Pain that continues despite using cushions, posture corrections, or over-the-counter medications.
- Pain interferes with daily life, work, or sleep.
Diagnosis and Evaluation by Doctors
If you visit a doctor, they may conduct:
- Physical Examination – Palpating the coccyx and surrounding muscles for tenderness.
- Imaging Tests – X-rays, MRI, or CT scans to detect fractures, dislocations, or tumors.
- Lab Tests – If infection or systemic disease is suspected.
Doctors may also inquire about lifestyle, occupation, medical history, and childbirth history in women to identify risk factors.
Diagnosis of Tailbone Pain
Accurate diagnosis is the cornerstone of effective treatment. Since tailbone pain (coccydynia) can arise from multiple causes ranging from simple trauma to rare tumors, a structured diagnostic approach is essential.
Initial Medical History
The diagnostic process usually begins with a comprehensive medical history, where a doctor asks questions such as:
- When did the pain start?
- Was it preceded by an injury, fall, or childbirth?
- Is the pain constant or only when sitting?
- Does pain radiate to other parts (hips, thighs, back)?
- Are there additional symptoms (fever, numbness, bowel/bladder issues)?
- Has the patient experienced weight changes, cancer history, or chronic illness?
This helps in distinguishing traumatic vs. non-traumatic causes [4].
Physical Examination
During a physical exam, a doctor may:
- Palpate the Coccyx – Press around the tailbone to locate tenderness or swelling.
- Rectal Examination – Sometimes done to check coccyx mobility and rule out tumors or cysts.
- Check Posture and Gait – Poor posture or spinal misalignment may contribute to pain.
- Neurological Testing – If nerve-related symptoms are present, reflexes and strength are evaluated.
Imaging Tests
- X-rays – Useful for detecting fractures, dislocations, or abnormal alignment of the coccyx.
- MRI (Magnetic Resonance Imaging) – Provides detailed images of soft tissues, ligaments, discs, and potential tumors.
- CT Scan – Used in complex cases where fine bone detail is required.
- Dynamic Sitting and Standing X-rays – Sometimes doctors compare coccyx alignment in different postures.
Differential Diagnosis
Tailbone pain can mimic or overlap with other conditions. Doctors rule out:
- Lumbar disc herniation or sciatica
- Sacral fractures
- Pelvic floor dysfunction
- Infections (pilonidal cyst, osteomyelitis)
- Tumors (benign or malignant in the pelvic region)
Management and Treatment Options
Treatment depends on the severity, duration, and underlying cause of coccyx pain. Most cases improve with conservative care, but persistent or severe cases may need medical procedures.
Home Remedies and Self-Care
These first-line strategies are often effective for mild to moderate coccyx pain:
- Coccyx Cushions (Donut or Wedge Cushions) – Reduce pressure on the tailbone when sitting.
- Heat Therapy – Heating pads relax muscles and improve blood flow.
- Cold Therapy – Ice packs help reduce inflammation and swelling after acute injuries.
- Rest and Position Changes – Avoid prolonged sitting; alternate between standing and walking.
- Over-the-Counter Pain Relievers – NSAIDs (ibuprofen, naproxen) reduce inflammation and discomfort.
Lifestyle Modifications
Adopting ergonomic and lifestyle changes can significantly reduce recurrence:
- Posture Correction – Keeping the back straight and shoulders relaxed while sitting.
- Frequent Breaks – Standing and stretching every 30–45 minutes during desk work.
- Weight Management – Reducing obesity-related coccyx pressure.
- Supportive Seating – Using ergonomic chairs that provide proper spinal alignment.
Physical Therapy and Rehabilitation
A physical therapist may guide exercises that strengthen surrounding muscles:
- Pelvic Floor Exercises – Improve support and reduce coccyx stress.
- Stretching of Gluteal and Hip Muscles – Relieves tension around the lower spine.
- Core Strengthening Exercises – Stabilizes the spine and reduces coccyx pressure.
- Manual Therapy – Includes massage, joint mobilization, or myofascial release.
Some therapists also use ultrasound therapy, electrical stimulation, or biofeedback to improve recovery.
Medical Treatments
If conservative measures fail, doctors may prescribe or perform:
- Prescription Medications – Stronger NSAIDs, muscle relaxants, or neuropathic pain medications.
- Steroid Injections – Corticosteroid injections reduce inflammation around sacrococcygeal joints.
- Nerve Blocks – Anesthetics injected around coccygeal nerves provide temporary or long-term relief.
Minimally Invasive and Surgical Procedures
Surgery is rarely needed, but it can be considered in chronic, disabling cases:
- Ganglion Impar Block – Targets nerve clusters transmitting coccyx pain.
- Radiofrequency Ablation – Destroys specific nerve fibers to stop pain signals.
- Coccygectomy (Tailbone Removal Surgery) – A last-resort option when all other treatments fail.
While effective in select cases, coccygectomy carries risks such as infection, wound healing problems, and persistent pain. Therefore, it is reserved only for severe, refractory cases.
Complementary and Alternative Therapies
Some patients find relief in additional approaches:
- Chiropractic Adjustments – Gentle spinal manipulations may reduce pain.
- Acupuncture – Stimulates specific points to relieve chronic coccyx pain.
- Yoga and Mind-Body Practices – Improve posture, flexibility, and stress reduction.
- Herbal Remedies – Anti-inflammatory herbs like turmeric or ginger may provide mild benefits, though evidence is limited.
Prevention Tips
Preventing tailbone pain is often easier than managing it after it occurs. Many strategies focus on maintaining proper posture, reducing strain, and adopting healthy lifestyle habits.
Correct Sitting Posture
Sitting posture plays a major role in coccyx health. To avoid unnecessary strain:
- Keep both feet flat on the ground.
- Sit with your hips and knees at a 90-degree angle.
- Avoid slouching, which tilts the pelvis and pushes pressure on the coccyx.
- Use lumbar support to maintain the spine’s natural curve.
Use of Coccyx Cushions
Special cushions (U-shaped, donut-shaped, or wedge cushions) can reduce pressure while sitting. These are especially beneficial for people who spend long hours at desks or who are recovering from childbirth or injury.
Regular Stretching and Exercise
Incorporating simple daily exercises can prevent stiffness and promote circulation:
- Pelvic tilts to strengthen the lower back.
- Hamstring stretches to reduce pelvic pulling.
- Core-strengthening workouts like planks for spinal stability.
- Yoga poses such as Child’s Pose or Cat-Cow for gentle spinal movement.
Avoiding Prolonged Sitting
Take breaks every 30–45 minutes during sedentary tasks. Standing up, walking, or stretching helps relieve coccyx pressure and improves blood flow [5].
Weight Management
Maintaining a healthy body weight reduces coccyx stress. Obesity increases coccyx pressure, while being underweight decreases natural fat padding. Both can contribute to pain.
Safe Practices During Pregnancy and Childbirth
Expecting mothers can lower their risk of coccyx pain by:
- Practicing gentle prenatal exercises.
- Using cushions while sitting.
- Discussing birthing positions with healthcare providers.
How Sitting Mechanics Affect the Coccyx
The coccyx plays a critical role in weight distribution during sitting. When sitting mechanics are poor such as leaning backward, slouching, or sitting on hard surfaces, excessive pressure is placed directly on the tailbone. This often results in coccyx pain while sitting and irritation of the sacrococcygeal joint.
Proper sitting mechanics shift load toward the sitting bones instead of the coccyx, offering effective sitting bone pain relief and reducing the risk of sacrococcygeal joint pain over time.
Acute vs Chronic Tailbone Pain
Tailbone pain can be classified based on duration and severity.
Acute tailbone pain usually follows a fall, childbirth, or sudden strain and often improves within weeks with rest and conservative care.
Chronic coccyx discomfort, on the other hand, persists for months and may be linked to posture issues, repetitive strain, or unresolved inflammation.
Understanding this distinction helps guide appropriate coccydynia treatment options and prevents long-term disability.
How Posture Influences Coccyx Stress
Posture has a direct impact on coccyx loading. Slouched sitting tilts the pelvis backward, increasing pressure on the coccyx and surrounding ligaments. Over time, this contributes to coccyx inflammation causes such as ligament strain and joint irritation.
Neutral spine alignment reduces coccyx stress, minimizes non-traumatic tailbone pain, and supports long-term pelvic and spinal health.
Role of Pelvic Floor Muscles in Coccydynia
The coccyx serves as an anchor point for pelvic floor muscles. Tightness, weakness, or imbalance in these muscles can lead to pelvic floor dysfunction pain, which often presents as tailbone discomfort.
Conditions such as chronic constipation, childbirth, or prolonged sitting may overload the pelvic floor, contributing to persistent coccydynia. Addressing pelvic floor health is therefore a key component of managing chronic coccyx discomfort.
Tailbone Pain After Falls and Minor Trauma
Even minor falls can bruise or misalign the coccyx. While fractures are less common, soft tissue injury and joint irritation frequently occur, leading to classic tailbone injury symptoms such as sharp pain when sitting or transitioning to standing.
Early care after falls helps prevent lingering sacrococcygeal joint pain and reduces the risk of pain becoming chronic.
Why Tailbone Pain Can Persist Without Injury
Not all coccyx pain follows trauma. In many cases, pain develops gradually due to prolonged sitting, poor posture, or muscle imbalance. This type of non-traumatic tailbone pain is often linked to repetitive micro-stress rather than a single injury.
Left unaddressed, these factors can sustain inflammation and lead to long-standing discomfort even in the absence of visible damage.
Impact of Sedentary Lifestyle on Coccyx Health
A sedentary lifestyle significantly increases coccyx strain. Long hours of sitting reduce blood flow, increase joint compression, and weaken supportive muscles.
Office workers, drivers, and students are particularly vulnerable to coccyx pain while sitting, making regular movement, posture correction, and ergonomic seating essential for prevention.
Conclusion
Tailbone pain (coccydynia) is a common yet often overlooked condition that can interfere with daily activities like sitting, standing, or walking. It can result from trauma, posture issues, childbirth, obesity, infections, or degenerative conditions.
The good news is that most cases improve with conservative treatment such as cushions, posture correction, exercises, and pain relievers. Medical care becomes essential if pain is severe, persistent, or linked to other symptoms such as fever, numbness, or sudden weight loss.
By combining prevention strategies, timely diagnosis, and individualized treatment, patients can achieve long-term relief and improve quality of life.
Looking for more health and wellness solutions ? Don’t miss these related guides:-
- Posture and ergonomics tips for pain relief prevent your muscles and joints from the wear and tear
- Is poor posture aging you faster
Frequently Asked Questions:
1. What are the most common reasons for tailbone pain?
The most common causes include falls or trauma, prolonged sitting on hard surfaces, poor posture, childbirth-related stress, obesity, and degenerative changes like arthritis. Rarely, infections or tumors may be involved.
2. Can sitting for long hours cause tailbone pain?
Yes. Prolonged sitting, especially on hard or poorly cushioned surfaces, increases pressure on the coccyx and can lead to inflammation and pain.
3. Why does my tailbone hurt after childbirth?
During delivery, the coccyx can be pushed backward, stretched, or bruised due to pressure from the baby’s head. Hormonal changes that loosen ligaments also make the coccyx more vulnerable.
4. How can obesity contribute to coccyx pain?
Excess body weight increases downward pressure on the coccyx. Conversely, being underweight reduces protective fat padding, which can also increase pain risk.
5. Is tailbone pain related to arthritis?
Yes. Degenerative arthritis in the sacrococcygeal joints can cause chronic tailbone pain, especially in older adults.
References:
- American Academy of Orthopaedic Surgeons. (2023). Coccyx (tailbone) pain. OrthoInfo. https://orthoinfo.aaos.org
- Foye, P. M. (2017). Coccydynia: Tailbone pain. Physical Medicine and Rehabilitation Clinics of North America, 28(3), 539–549. https://www.sciencedirect.com/science/article/abs/pii/S1047965117300244
- Maigne, J. Y., Doursounian, L., & Chatellier, G. (2000). Causes and mechanisms of common coccydynia: Role of body mass index and coccygeal trauma. Spine, 25(23), 3072–3079. https://journals.lww.com/spinejournal/abstract/2000/12010/causes_and_mechanisms_of_common_coccydynia__role.15.aspx
- Postacchini, F., & Massobrio, M. (1983). Idiopathic coccygodynia: Analysis of fifty-one operative cases and a radiographic study of the normal coccyx. Journal of Bone and Joint Surgery, 65(8), 1116–1124. https://journals.lww.com/jbjsjournal/abstract/1983/65080/idiopathic_coccygodynia__analysis_of_fifty_one.11.aspx
- Shaladi, A. M., Marinangeli, F., & Varrassi, G. (2012). Treatment of chronic coccydynia with radiofrequency thermocoagulation. Pain Practice, 12(2), 148–153. https://onlinelibrary.wiley.com/doi/10.1111/j.1533-2500.2011.00472.x