For a long time, mental health has been treated as a problem of thoughts. Change the mindset. Reframe the narrative. Think more positively. But quietly, beneath all that effort, another system has been shaping how you feel long before a single thought appears.
Your gut.
Research into the gut–brain connection has revealed something unexpected. People struggling with anxiety, low mood, poor sleep, or constant emotional unease often share a common underlying issue: compromised gut health. Chronic gut inflammation, food sensitivities, microbiome imbalance, or a weakened gut lining show up repeatedly.
Their minds were not broken.
Their bodies were signaling distress.
And the gut was not subtle about it.
What Science Says About the Gut–Brain Connection
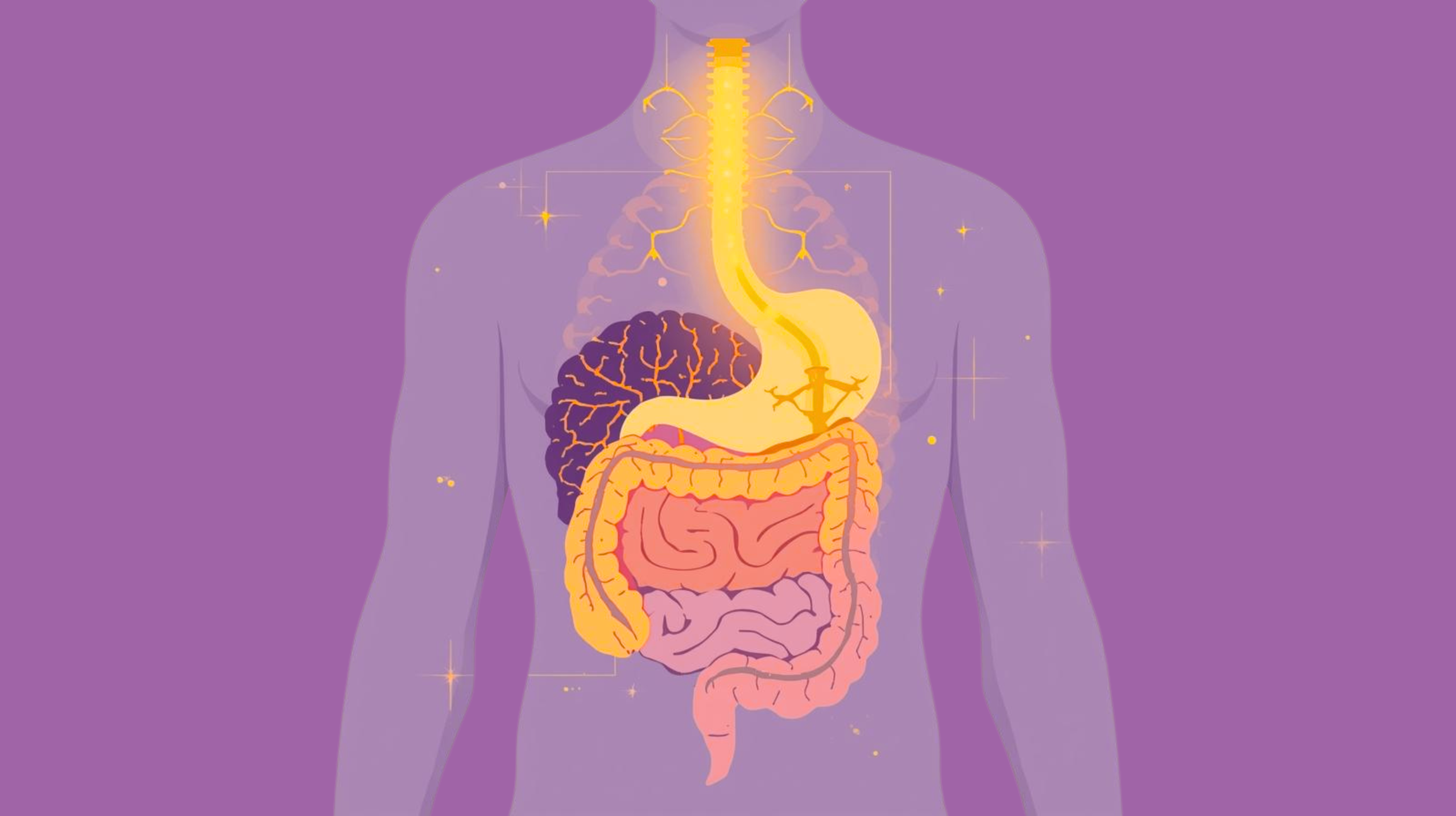
The gut and brain are in constant two-way communication through the gut–brain axis, a complex network involving the vagus nerve, immune system, hormones, and neurotransmitters.
Your gut houses trillions of bacteria, collectively called the microbiome. These microbes play a direct role in mood regulation, stress response, and emotional balance. Studies show that disturbances in the microbiome are strongly associated with anxiety, depression, and sleep disorders.
This means gut health and mental health are inseparable. When digestion is inflamed or imbalanced, emotional regulation becomes harder, even if life circumstances are stable.
Your Gut Is Not Just Digestive. It Is Emotional.
Nearly 90% of serotonin production in the gut happens outside the brain. Serotonin is not just the “happy chemical.” It governs sleep quality, emotional resilience, motivation, and the body’s sense of safety.
When the gut is healthy:
- Serotonin signaling remains stable
- The nervous system feels regulated
- Emotional responses feel proportionate
When the gut is inflamed:
- Serotonin signaling becomes erratic
- The brain receives mixed safety signals
- Anxiety, restlessness, and low mood emerge
This is why digestive health and emotions are deeply intertwined.
How Gut Health Affects Anxiety, Mood, and Sleep
Gut Inflammation and Anxiety
Chronic gut irritation activates immune responses that release inflammatory molecules. These molecules can cross the blood–brain barrier and stimulate stress circuits, leading to gut inflammation and anxiety that feels persistent and hard to explain.
Microbiome and Mood
Certain gut bacteria produce compounds that calm the nervous system. When these bacteria decline, mood stability declines with them. An imbalanced microbiome often shows up as irritability, emotional sensitivity, or brain fog.
Gut Health and Sleep Quality
Poor digestion disrupts serotonin and melatonin balance, affecting sleep depth and recovery. People with gut issues often sleep but wake feeling unrefreshed, highlighting the link between gut health and sleep quality.
When the Gut Feels Unsafe, So Do You
Conditions like leaky gut and mental health disturbances go hand in hand. When the gut lining becomes permeable, inflammatory compounds leak into circulation, triggering stress responses in the brain.
The result is not dramatic panic. It is quieter:
- A constant background anxiety
- Difficulty relaxing at night
- Emotional fragility
- Low mood without a clear cause
Your nervous system stays alert because your body is signaling internal danger.
The Stress and Digestion Connection
Stress doesn’t just affect your thoughts. It alters stomach acid, slows digestion, changes gut bacteria, and weakens the gut lining. This creates a feedback loop:
Stress → poor digestion
Poor digestion → inflammation
Inflammation → nervous system activation
Nervous system activation → more stress
This loop explains why mental health challenges often persist despite mindset work alone.
Signs Your Mental Health May Be Gut-Driven
- Mood shifts after meals
- Anxiety without obvious triggers
- Feeling emotionally “off” for no reason
- Sleep that feels shallow or unrefreshing
- Sugar or comfort-food cravings for emotional stability
- Brain fog or fatigue linked to digestion
These are not personality traits. They are biological signals asking for regulation.
Everyday Habits That Damage Gut-Brain Balance
You don’t need a diagnosis for gut–brain disruption. Small daily habits are enough:
- Eating while stressed or distracted
- Skipping meals or eating erratically
- Excessive ultra-processed foods
- Using caffeine to override exhaustion
- Ignoring bloating, acidity, or discomfort
Each habit communicates unsafety to the gut. The gut responds with inflammation. The brain responds with vigilance.
How to Support Gut Health for Better Mental Wellbeing
Improving gut health is not about extreme diets or control. It is about restoring safety.
Key foundations:
- Eat regular, balanced meals
- Prioritize whole, minimally processed foods
- Reduce inflammatory triggers
- Respect digestion instead of pushing through discomfort
When the gut calms, the nervous system and gut health recalibrate together.
Simple Daily Practices to Support Gut–Brain Health
- Eat slowly and without screens
- Include fiber-rich foods to support the microbiome
- Stay hydrated to protect gut lining
- Get consistent sleep to regulate digestion
- Manage stress with gentle movement or breathwork
Consistency matters more than perfection.
Healing Starts With Safety, Not Control
Supporting gut health is not about forcing discipline. It is about reducing threat signals in the body.
When digestion feels safe:
- Serotonin stabilizes
- The nervous system softens
- Mood regulation improves naturally
Mental clarity returns not because you “thought better,” but because your body stopped sending distress signals.
The Real Takeaway
Mental health does not begin in the mind alone. It begins in the body systems that decide whether you feel safe enough to rest, connect, and think clearly.
Your gut doesn’t whisper.
It writes your emotional headlines daily.
If your mood, sleep, or emotional balance feels fragile, the question may not be what you’re thinking wrong but what your body is struggling to process.
Because sometimes, healing the mind starts by listening below the neck.
Co- authored by: Shayamal Vallabhjee
Chief Science Officer: betterhood
Shayamal is a Human Performance Designer who works at the intersection of psychology, physiology, and human systems design, for the last 25 years he is helping high-performing leaders, teams, and athletes thrive in environments of stress, complexity, and change. His work spans across elite sports, corporate leadership, and chronic health—and is grounded in the belief that true performance isn’t about pushing harder, but designing better.
Frequently Asked Questions (FAQs)
1. How does gut health affect mental health?
Gut health influences neurotransmitter production, inflammation levels, and nervous system regulation. Poor gut health can directly contribute to anxiety, low mood, and sleep disturbances.
2. Can gut inflammation cause anxiety or low mood?
Yes. Gut inflammation activates immune pathways that affect the brain, increasing stress sensitivity and emotional instability.
3. What are signs of poor gut–brain connection?
Persistent anxiety, mood changes after meals, brain fog, poor sleep, digestive discomfort, and sugar cravings are common signs.
4. Can improving gut health help with sleep?
Yes. Balanced gut function supports serotonin and melatonin production, improving sleep quality and recovery.
5. How long does it take to see mental health changes after improving gut health?
Some people notice changes within days, especially if symptoms are food-related. Deeper healing may take several weeks of consistent gut support.