Inflammation is the body’s natural defense mechanism: a complex immune response that mobilizes white blood cells, cytokines, and other factors to repair damage and fight infection. In its acute form, inflammation is beneficial, it helps heal wounds, clear pathogens, and restore balance.
Sleep is not just downtime. It is an active, regenerative state wherein immune, metabolic, and neurological systems reset [1]. Good quality sleep helps regulate hormones, clear metabolic waste, and maintain immune balance.
Unfortunately, our 24/7 culture, screen overexposure, work stress, and erratic schedules have normalized sleep restriction and disruption. Over time, chronic poor sleep becomes a silent driver of systemic inflammation and disease.
In this article, we’ll examine how poor sleep triggers inflammation, the health consequences, the scientific evidence, and practical ways to reverse this harmful cycle.
Understanding Inflammation: The Body’s Defense Mechanism
Acute vs. Chronic Inflammation
- Acute inflammation is short-term, localized, and helpful (e.g., swelling around a cut).
- Chronic inflammation is a low-grade, persistent immune activation that damages tissues and fuels disease.
How Acute Inflammation Helps
When you get injured or infected, immune cells release cytokines (e.g., IL-1, IL-6, TNF-α), attract other immune cells, increase blood flow, and clear pathogens or debris. After the threat resolves, inflammation subsides, and healing occurs.
How Chronic Inflammation Harms
When inflammation fails to shut off, it can:
- Damage tissues and organs (e.g. arteries, joints, brain)
- Promote fibrosis or scarring
- Impair insulin signaling
- Disrupt cellular repair
- Increase risk of chronic diseases (cardiovascular, metabolic, neurodegenerative)
Inflammatory Markers
- C-reactive protein (CRP): A liver-produced protein that rises in response to inflammation [2].
- Interleukin-6 (IL-6): A multifunctional cytokine that both drives and regulates inflammation.
- Tumor Necrosis Factor–alpha (TNF-α): A key cytokine that amplifies immune responses.
These markers are often measured in blood tests to assess systemic inflammation.
Link to Sleep Quality
Emerging research shows that sleep quality and patterns influence levels of CRP, IL-6, and TNF-α. Poor sleep can upregulate these markers, tipping the balance toward chronic inflammation. We will explore this in depth.
The Science of Sleep and Its Role in Health
1. Sleep Stages: REM and Non-REM
Sleep cycles through stages:
- Non-REM (N1 → N2 → N3 / slow-wave sleep): Deep, restorative sleep, crucial for growth, repair, and immune regulation.
- REM (Rapid Eye Movement): Dreaming sleep, involved in emotional processing and neural plasticity.
Each night, your body oscillates through these stages. Disruption to this cycle impairs restorative functions [3].
2. Circadian Rhythm & Biological Regulation
Your circadian clock is an internal 24-hour timer regulating hormone release, metabolism, body temperature, and immune function. When your sleep timing is misaligned (e.g. shift work, irregular sleep), the clock and immune signals desynchronize, creating inflammatory imbalance.
3. Deep Sleep, Immune Balance & Cell Repair
Deep (slow-wave) sleep is essential for:
- Suppressing pro-inflammatory signaling
- Promoting anti-inflammatory cytokines
- DNA repair, protein synthesis
- Glymphatic clearance (waste elimination in brain)
When deep sleep is curtailed, immune dysregulation and inflammation follow.
4. Melatonin’s Anti-Inflammatory Role
Melatonin, produced in darkness, is more than a sleep hormone. It has antioxidant and anti-inflammatory properties, helping modulate immune response, reduce oxidative damage, and suppress inflammatory cytokines.
5. Sleep as a “Natural Healing State”
In ideal sleep, your body shifts into repair mode: inflammation is dampened, damage is repaired, and immune balance is restored. Poor or fragmented sleep disrupts this healing state, extending inflammatory activation into waking hours [4].
How Poor Sleep Triggers Inflammation
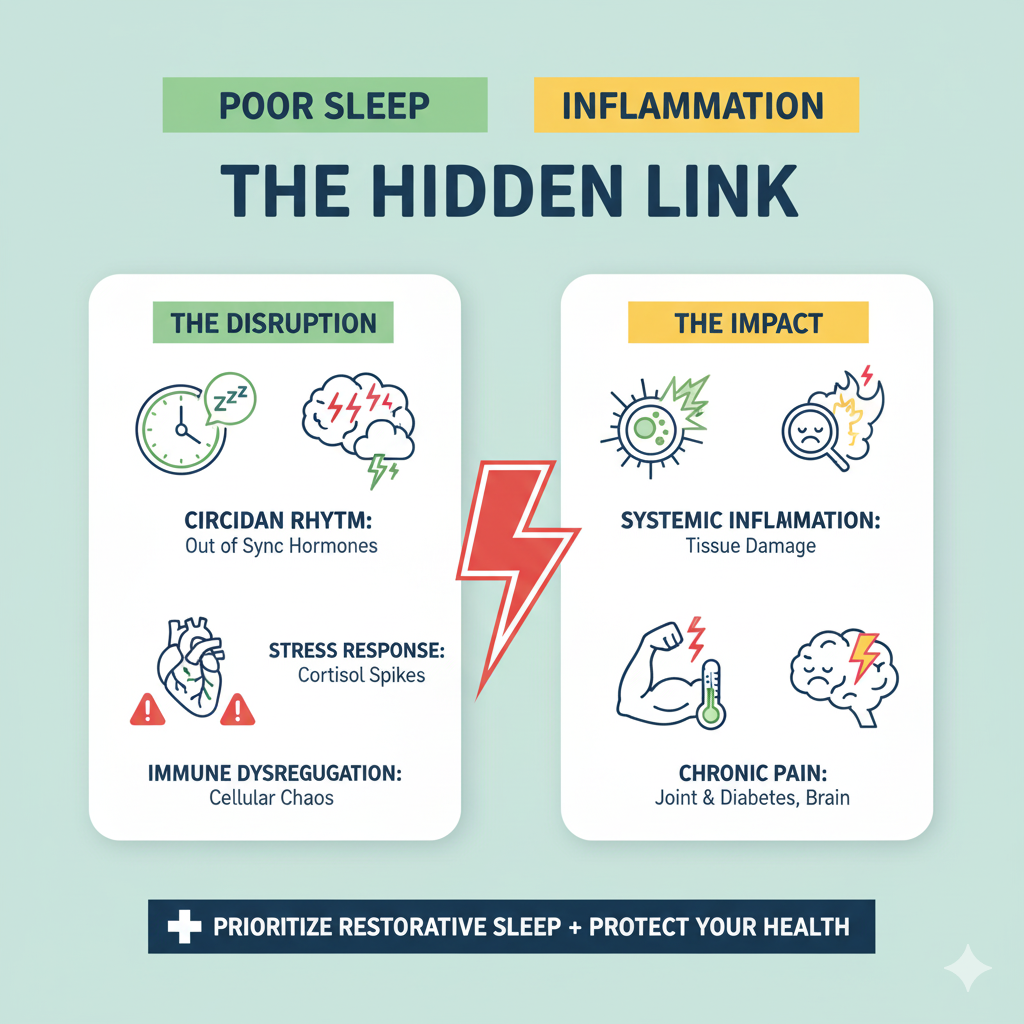
Now let’s see how insufficient or disrupted sleep leads to inflammation.
1. Activation of Stress Hormones
Poor sleep elevates cortisol and epinephrine (adrenaline) from the hypothalamic-pituitary-adrenal (HPA) axis. These stress hormones stimulate inflammatory pathways (e.g., NF-κB activation) that increase cytokine production.
2. Overactive Immune Response
Sleep deprivation induces higher levels of IL-6, TNF-α, and CRP. These pro-inflammatory cytokines can persistently remain elevated, fueling chronic inflammation.
- For example, restricting sleep to 50% of habitual time over 10 days significantly increased IL-6 levels.
- Experimental partial sleep deprivation over multiple nights was associated with higher IL-6 and CRP in healthy adults.
3. Disrupted Circadian Rhythm
Irregular sleep patterns confuse timing cues for immune cells [5]. Immune signaling is best when aligned with circadian rhythm; misalignment causes maladaptive inflammatory responses.
4. Reduced Melatonin Production
If sleep is delayed or suppressed, melatonin production falls. With less melatonin, the body loses a natural anti-inflammatory moderator, enabling unchecked cytokine activity.
5. Oxidative Stress and Cellular Damage
Lack of sleep increases reactive oxygen species (ROS) and oxidative damage to lipids, proteins, and DNA. This damage triggers inflammatory repair mechanisms, further burdening the immune system.
Health Consequences of Sleep-Related Inflammation
Chronic inflammation driven by poor sleep contributes to a host of health problems:
1. Cardiovascular Diseases
Elevated CRP is a known risk marker for heart disease, atherosclerosis, and stroke. Poor sleep elevates CRP and other inflammatory mediators, increasing cardiovascular risk.
2. Metabolic & Endocrine Disorders
Inflammation impairs insulin signaling and promotes metabolic syndrome, obesity, and type 2 diabetes. Sleep loss worsens glucose tolerance and fat accumulation.
3. Neuroinflammation & Mental Health
Persistent inflammation in the brain is linked to depression, anxiety, and Alzheimer’s disease [6]. Sleep disruption accelerates neuroinflammatory processes, reduces clearance of toxic proteins, and damages cognition.
4. Weakened Immune System
Overactive inflammation paradoxically blunts immune responsiveness over time leading to greater susceptibility to infections and slower recovery.
5. Accelerated Aging & Oxidative Damage
Chronic inflammation shortens telomeres (protective chromosome caps), promotes cellular senescence, and accelerates biological aging. Sleep deprivation fosters oxidative stress and speeds this process.
What Research Says: Scientific Evidence
Let’s look at key studies that demonstrate the link between sleep and inflammation.
1. Irwin et al. (Systematic Review & Meta-Analysis, 2015)
This meta-analysis of 72 studies (n > 50,000) found that sleep disturbance was associated with significantly higher levels of CRP and IL-6.
Short sleep duration had a weaker, but present, association with CRP, though not always with IL-6.
2. Experimental Sleep Deprivation Studies
- In a controlled 10-day protocol, partial sleep restriction (4 hours/night) increased IL-6 significantly.
- Acute total sleep deprivation over 40 hours triggered elevated IL-6 and CRP in some studies.
- A recent meta-analysis (2025) found that partial sleep deprivation over multiple nights (3+ nights) significantly raised peripheral IL-6 and CRP levels, while a single night alone didn’t show significant changes.
3. Immune Regulation and Cytokine Balance
Besedovsky’s work (2012) and others highlight that sleep modulates cytokine cross-talk, T-cell function, and immune homeostasis. Sleep loss disrupts this regulatory balance, pushing cytokines upward.
4. Miller & Cappuccio and Others
Many epidemiologic studies link short or poor sleep with markers of inflammation, obesity, metabolic disease, and cardiovascular risk. Although causality is complex, the consistent associations support the biological plausibility.
5. Summary of Findings
Across experimental and observational work, a consistent link exists between poor sleep and elevated inflammatory markers such as CRP and IL-6. The effect is stronger with prolonged partial deprivation and persistent sleep disturbances.
Reducing Inflammation Through Better Sleep
Now that we understand the mechanisms, let’s look at actionable strategies to reverse and prevent sleep-driven inflammation.
1. Maintain a Consistent Sleep Schedule
Go to bed and wake up at the same time daily even on weekends. This strengthens your circadian cues and optimizes immune timing.
2. Create a Relaxing Sleep Environment
- Make your bedroom dark, cool (~18–20 °C), and quiet.
- Limit screens before bed to reduce blue light interference with melatonin.
- Use blackout curtains, eye masks, or white noise if necessary.
3. Follow an Anti-Inflammatory Diet
Foods that help reduce inflammation include:
- Omega-3-rich fish (salmon, mackerel)
- Berries, leafy greens, nuts
- Turmeric, ginger, green tea
- Whole grains, legumes
Avoid processed foods, excess refined sugar, and trans fats. A healthy diet supports both sleep quality and inflammation control [6].
4. Manage Stress & Emotions
Chronic psychological stress elevates cortisol, which drives inflammation. Incorporate:
- Meditation, mindfulness
- Deep breathing or alternate nostril breathing
- Yoga, tai chi, stretching
- Journaling or expressive writing
These practices help reduce stress load, enabling better sleep and lower inflammation.
5. Limit Stimulants & Alcohol
- Avoid caffeine 6–8 hours before bedtime
- Quit nicotine (if applicable)
- Avoid using alcohol as a sleep aid, it fragments sleep and increases inflammation.
6. Exercise Regularly but Not Too Late
Regular moderate exercise (aerobic + resistance) helps regulate immune function and enhances sleep.
Try to finish vigorous workouts at least 2–3 hours before bedtime to avoid sleep disruption.
7. Seek Professional Help When Necessary
If insomnia, obstructive sleep apnea, or chronic sleep trouble persist, consult a sleep specialist, pulmonologist, or physician [7]. Treating underlying sleep disorders is crucial for breaking the inflammation loop.
Holistic and Natural Approaches
Beyond the core strategies above, some supportive, gentle methods can further aid your sleep-inflammation balance:
1. Alternative Methods
- Aromatherapy (lavender, chamomile) can help induce calm
- Herbal teas (e.g. chamomile, valerian) in moderation and under supervision
- Mindfulness, guided imagery, sound baths for relaxation
2. Supplements (with Medical Oversight)
Some supplements may support sleep and inflammation reduction only under physician guidance:
- Magnesium (often magnesium glycinate) to promote relaxation
- Ashwagandha or adaptogens (careful with effects on cortisol)
- Melatonin (low dose, short-term) for circadian support
- Omega-3 supplements if dietary intake is inadequate
Always consult your doctor before starting supplements, especially if on medications or with health conditions [8].
3. Balanced Lifestyle Integration
The most sustainable approach is integration:
- Pair an anti-inflammatory diet with sleep hygiene
- Combine stress management practices with consistency
- Move your body, nourish it, rest it and treat each aspect as interconnected
Healing inflammation through sleep is rarely about a single “magic fix”, it’s about layered habits over time.
Conclusion
Sleep isn’t optional, it’s a core pillar of health. Poor sleep fuels a cascade of inflammatory processes that can quietly undermine your immune system, metabolic health, cardiovascular integrity, and brain function.
But the hopeful message is this: many of these harmful pathways are reversible. By restoring high-quality, consistent sleep, managing stress, aligning your lifestyle, and seeking help when needed, you can dampen inflammation, restore balance, and protect your long-term health.
Focus on sleep as your nightly opportunity for healing, your body’s immune system, metabolism, and organs will thank you.
Looking for more health and wellness solutions? Don’t miss these related guides:-
Frequently Asked Questions:
1. What is the connection between poor sleep and inflammation?
Poor or fragmented sleep increases stress hormones, elevates cytokines (IL-6, TNF-α), reduces melatonin’s anti-inflammatory action, and leads to oxidative damage cumulatively pushing the body into chronic inflammation.
2. How does lack of sleep affect the immune system?
Chronic sleep loss dysregulates immune signaling, impairs T-cell function, and reduces immune resilience, making you more susceptible to infections and slower to recover.
3. Can poor sleep increase the risk of chronic diseases?
Yes. Sleep-related inflammation is implicated in cardiovascular disease, metabolic syndrome, diabetes, neurodegenerative disease, and accelerated aging.
4. How long does it take to reduce inflammation after improving sleep?
It depends on baseline health and duration of disruption. Some inflammatory markers respond within days to weeks of improved sleep; sustained changes often require months of consistent habits.
5. What are common signs of inflammation caused by sleep deprivation?
Persistent fatigue, joint or muscle pain, elevated resting heart rate, mood disturbances, poor recovery from workouts, frequent infections, and biomarkers (high CRP, IL-6) on blood tests.
References
- Irwin MR, Olmstead R, Carroll JE. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC4666828
- Patel SR, Zhu X, Storfer-Isser A, et al. Sleep duration and biomarkers of inflammation. Sleep.https://pmc.ncbi.nlm.nih.gov/articles/PMC2635584
- Meier-Ewert HK, Ridker PM, et al. Effect of sleep loss on C-Reactive protein, an inflammatory marker. JACC. https://www.med.upenn.edu/uep/assets/user-content/documents/Meier-Ewert2004CReactive.pdf
- Study on prolonged sleep restriction (10 days) increasing IL-6. https://pmc.ncbi.nlm.nih.gov/articles/PMC1978405/
- Effects of experimental partial sleep deprivation on IL-6 and CRP (multi-night protocols). https://pubmed.ncbi.nlm.nih.gov/40474574/
- The role of inconsistent sleep and inflammatory markers like IL-6, https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2020.01042/
- Nature article: sleep deprivation and immune-disease risk. https://www.nature.com/articles/s42003-021-02825-4
- Harvard Health: how sleep deprivation can cause inflammation. https://www.health.harvard.edu/healthbeat/how-sleep-deprivation-can-cause-inflammation